Heartburn is a common digestive issue that causes a burning sensation in the chest, often after eating. It occurs when stomach acid flows back into the esophagus, irritating its lining. While occasional heartburn is harmless, frequent episodes may indicate acid reflux or Gastroesophageal Reflux Disease (GERD).
Several factors contribute to heartburn, including diet, lifestyle, and underlying medical conditions. Spicy foods, caffeine, stress, and poor eating habits can all trigger discomfort. Fortunately, by identifying triggers and making simple adjustments, you can reduce or even prevent heartburn.
In this article, we’ll explore the main causes of heartburn, how your lifestyle plays a role, and the best ways to prevent and treat it effectively.
Common Causes of Heartburn
Spicy and Acidic Foods – How They Trigger Heartburn
Certain foods are known to irritate the esophagus and weaken the lower esophageal sphincter (LES), the muscle responsible for keeping stomach acid from rising into the esophagus. Among the biggest culprits are spicy and acidic foods, which can increase stomach acid production and cause heartburn symptoms.
1. Spicy Foods
Spicy dishes containing chili peppers, hot sauces, and strong seasonings like black pepper and cayenne can trigger heartburn by irritating the esophageal lining. Capsaicin, the compound that gives chili peppers their heat, can slow digestion, keeping food in the stomach longer and increasing the risk of acid reflux.
2. Acidic Foods
Acidic foods have a low pH, which can increase acidity in the stomach and irritate an already sensitive esophagus. Common acidic foods that trigger heartburn include:
- Tomatoes and tomato-based products (sauces, ketchup, salsa)
- Citrus fruits like oranges, lemons, grapefruits, and limes
- Vinegar-based dressings and pickled foods
3. How to Reduce Heartburn from These Foods
If you experience frequent heartburn, you don’t have to eliminate these foods entirely. Instead, try:
- Eating smaller portions to reduce acid buildup.
- Pairing acidic foods with alkaline options like leafy greens, bananas, or whole grains.
- Using milder seasonings like herbs (basil, oregano) instead of spicy chilies.
- Avoiding eating these foods close to bedtime to prevent reflux when lying down.
By being mindful of your diet, you can still enjoy flavorful meals while reducing the risk of heartburn.
Overeating and Late-Night Eating – How They Trigger Acid Reflux
The way you eat is just as important as what you eat when it comes to preventing heartburn. Overeating and eating too close to bedtime are two of the most common habits that contribute to acid reflux and discomfort. These behaviors put extra pressure on the stomach, making it easier for stomach acid to flow back into the esophagus.
1. How Overeating Causes Heartburn
When you eat large meals, your stomach stretches to accommodate the extra food. This increases pressure on the lower esophageal sphincter (LES), the muscle that prevents stomach acid from rising. If the LES becomes weak or overly strained, acid can escape into the esophagus, leading to a burning sensation in the chest.
Common overeating mistakes that trigger heartburn:
- Eating large portions in one sitting – Overloading the stomach makes it harder to digest food properly.
- Consuming high-fat or greasy meals – Fat slows down digestion, keeping food in the stomach longer.
- Eating too quickly – Fast eating leads to swallowing excess air, causing bloating and increased stomach pressure.
2. The Impact of Late-Night Eating
Eating close to bedtime is another major trigger for acid reflux. When you lie down after a meal, gravity is no longer helping to keep stomach acid down, making reflux more likely. Additionally, the body’s digestion slows during sleep, which means food stays in the stomach longer.
Common late-night eating mistakes:
- Eating less than 2-3 hours before bed – This doesn’t allow enough time for digestion.
- Snacking on trigger foods – Spicy, acidic, or fatty foods worsen reflux when eaten late at night.
- Lying down immediately after eating – This increases the likelihood of acid backing up into the esophagus.
3. Tips to Avoid Heartburn from Overeating and Late-Night Eating
- Eat smaller, more frequent meals instead of large portions.
- Finish eating at least 3 hours before bedtime to allow for proper digestion.
- Choose lighter, low-acid snacks at night if you must eat (e.g., bananas, oatmeal, yogurt).
- Practice mindful eating – chew slowly and stop eating when you’re full.
- Stay upright after meals – take a light walk or sit up to help food digest properly.
By making these simple adjustments, you can prevent acid reflux and enjoy more comfortable digestion.
Alcohol and Caffeine – How These Beverages Relax the Lower Esophageal Sphincter (LES)
Both alcohol and caffeine are known to contribute to heartburn by relaxing the lower esophageal sphincter (LES), the muscle that acts as a barrier between the stomach and the esophagus. When this muscle weakens or relaxes too much, stomach acid can flow back up into the esophagus, causing acid reflux and heartburn symptoms.
1. How Alcohol Triggers Heartburn
Alcohol affects the digestive system in multiple ways that make heartburn more likely:
- Weakens the LES: Alcohol relaxes the LES, making it easier for stomach acid to escape into the esophagus.
- Increases stomach acid production: Some types of alcohol, such as wine and beer, stimulate excess acid secretion, heightening the risk of acid reflux.
- Irritates the esophageal lining: Alcohol can make the esophagus more sensitive to stomach acid, increasing discomfort.
- Slows digestion: Heavy alcohol consumption can slow gastric emptying, keeping food in the stomach longer and increasing pressure on the LES.
Worst alcoholic beverages for heartburn:
- Red and white wine (high acidity)
- Beer (carbonation increases bloating and pressure)
- Spirits with mixers (sugary and acidic ingredients worsen reflux)
2. How Caffeine Contributes to Acid Reflux
Caffeinated beverages can also contribute to heartburn, especially when consumed in large amounts. Here’s how:
- Relaxes the LES: Like alcohol, caffeine can weaken the LES, making it easier for stomach acid to rise into the esophagus.
- Increases stomach acid production: Coffee and energy drinks stimulate acid secretion, which can aggravate heartburn.
- Triggers acid reflux symptoms in some people: While not everyone experiences heartburn from caffeine, those who are prone to acid reflux may be more sensitive to its effects.
Worst caffeinated drinks for heartburn:
- Coffee (high caffeine and acidity)
- Black tea (contains caffeine and tannins that may irritate the stomach)
- Energy drinks (high caffeine content plus carbonation)
- Soda (combines caffeine, carbonation, and acidity, making it a triple threat)
3. Tips to Reduce Heartburn from Alcohol and Caffeine
If you struggle with heartburn but don’t want to completely give up alcohol or caffeine, try these strategies:
- Limit intake: Reduce consumption or switch to decaffeinated coffee and herbal teas.
- Drink in moderation: Stick to smaller portions, and avoid drinking on an empty stomach.
- Choose low-acid options: Opt for cold brew coffee (less acidic than hot coffee) or white wine over red wine (lower acidity).
- Stay hydrated: Drink water alongside alcohol or caffeine to dilute stomach acid.
- Drink earlier in the day: Avoid alcohol and caffeine in the evening to prevent late-night reflux.
By making these adjustments, you can still enjoy your favorite beverages while reducing the risk of heartburn and acid reflux.
Smoking and Tobacco Use – Their Impact on Stomach Acid Production and LES Function
Smoking and tobacco use are major contributors to acid reflux and heartburn because they affect both the lower esophageal sphincter (LES) and stomach acid production. The chemicals in cigarettes and tobacco can weaken the body’s ability to keep stomach acid in check, leading to frequent acid reflux episodes.
1. How Smoking Weakens the Lower Esophageal Sphincter (LES)
The LES is the muscle that prevents stomach acid from flowing back into the esophagus. When functioning properly, it remains tightly closed, opening only when you swallow. However, nicotine in cigarettes and other tobacco products directly affects LES function by:
- Relaxing the LES, making it easier for stomach acid to rise into the esophagus.
- Reducing saliva production, which is important because saliva neutralizes acid and helps wash it back down into the stomach.
- Delaying gastric emptying, meaning food stays in the stomach longer, increasing pressure on the LES and raising the risk of reflux.
2. The Effects of Smoking on Stomach Acid Production
Smoking also alters the stomach’s natural acid balance, leading to more frequent and severe heartburn:
- Increases stomach acid production – Nicotine stimulates acid secretion, worsening acid reflux symptoms.
- Irritates the esophageal lining – Smoke and toxic chemicals inflame the esophagus, making it more sensitive to stomach acid.
- Reduces bicarbonate secretion – The body produces bicarbonate to neutralize stomach acid, but smoking reduces this protective function.
3. Additional Ways Tobacco Use Worsens Acid Reflux
Beyond smoking, other forms of tobacco use (chewing tobacco, cigars, and vaping) also contribute to acid reflux and heartburn:
- Chewing tobacco increases stomach acid production and irritates the esophagus.
- Cigars have high nicotine content, causing even greater LES relaxation.
- Vaping may expose the esophagus to chemicals that trigger inflammation and worsen acid reflux.
4. How to Reduce Heartburn Caused by Smoking
Quitting smoking is the best way to reduce acid reflux, but if quitting is difficult, consider these strategies:
- Reduce smoking gradually to ease LES function recovery.
- Stay upright after smoking to prevent acid from rising.
- Chew sugar-free gum to increase saliva production and neutralize stomach acid.
- Limit alcohol and caffeine intake as they can worsen the effects of nicotine on the LES.
- Use nicotine replacement therapy (NRT) to reduce direct LES relaxation from smoking.
Smoking and tobacco use not only contribute to heartburn but also increase the risk of developing GERD (Gastroesophageal Reflux Disease) and esophageal damage over time. Quitting or reducing tobacco use can greatly improve digestion, LES function, and overall gut health, leading to fewer acid reflux episodes and better long-term well-being
How Your Lifestyle Affects Heartburn
Poor Posture After Eating – How Slouching or Lying Down Worsens Acid Reflux
Posture plays a significant role in digestion and acid reflux. The position of your body after eating can either help keep stomach acid in place or make it easier for it to flow back into the esophagus, leading to heartburn. Slouching, reclining, or lying down too soon after a meal can increase the likelihood of acid reflux and discomfort.
1. How Slouching Affects Digestion and Acid Reflux
When you slouch while sitting or standing after eating, you put extra pressure on your stomach, which can push acid up into the esophagus. This happens because:
- Compression of the stomach – Slouching compresses the abdomen, increasing pressure inside the stomach and forcing acid upward.
- Weakened lower esophageal sphincter (LES) function – Poor posture puts stress on the LES, making it easier for stomach acid to escape.
- Slower digestion – Hunched-over positions can slow gastric emptying, leading to prolonged acid buildup.
Common bad postures that trigger acid reflux:
- Sitting hunched over a desk or table after a meal.
- Leaning forward while working on a laptop or phone.
- Sitting with poor back support, causing abdominal compression.
2. Why Lying Down After Eating Causes Heartburn
Lying down too soon after a meal is one of the most common triggers of acid reflux because it removes the natural advantage of gravity in keeping stomach acid where it belongs. Here’s why:
- Gravity helps keep stomach acid down – When standing or sitting upright, gravity assists in digestion by keeping food and stomach acid moving downward.
- Lying down allows acid to travel up – Without gravity’s help, stomach acid can more easily move back into the esophagus, especially if the LES is weak.
- Digestion slows in a reclined position – This increases the time stomach acid stays in contact with the esophagus.
Worst positions for acid reflux after eating:
- Lying flat on your back or stomach right after a meal.
- Reclining on a couch or bed soon after eating.
- Sleeping on your right side (which can worsen reflux).
3. Best Posture Tips to Prevent Heartburn
To reduce the risk of acid reflux after eating, try these posture-friendly habits:
- Stay upright for at least 2-3 hours after meals – This allows food to digest properly before lying down.
- Sit with good posture – Keep your back straight and shoulders relaxed to avoid stomach compression.
- Take a light walk after eating – Gentle movement helps digestion and reduces acid buildup.
- Elevate your upper body while sleeping – If you experience nighttime reflux, try using a wedge pillow or raising the head of your bed by 6-8 inches.
- Sleep on your left side – This position helps keep stomach acid lower in the stomach and away from the esophagus.
By maintaining good posture and staying upright after meals, you can significantly reduce acid reflux and promote better digestion.
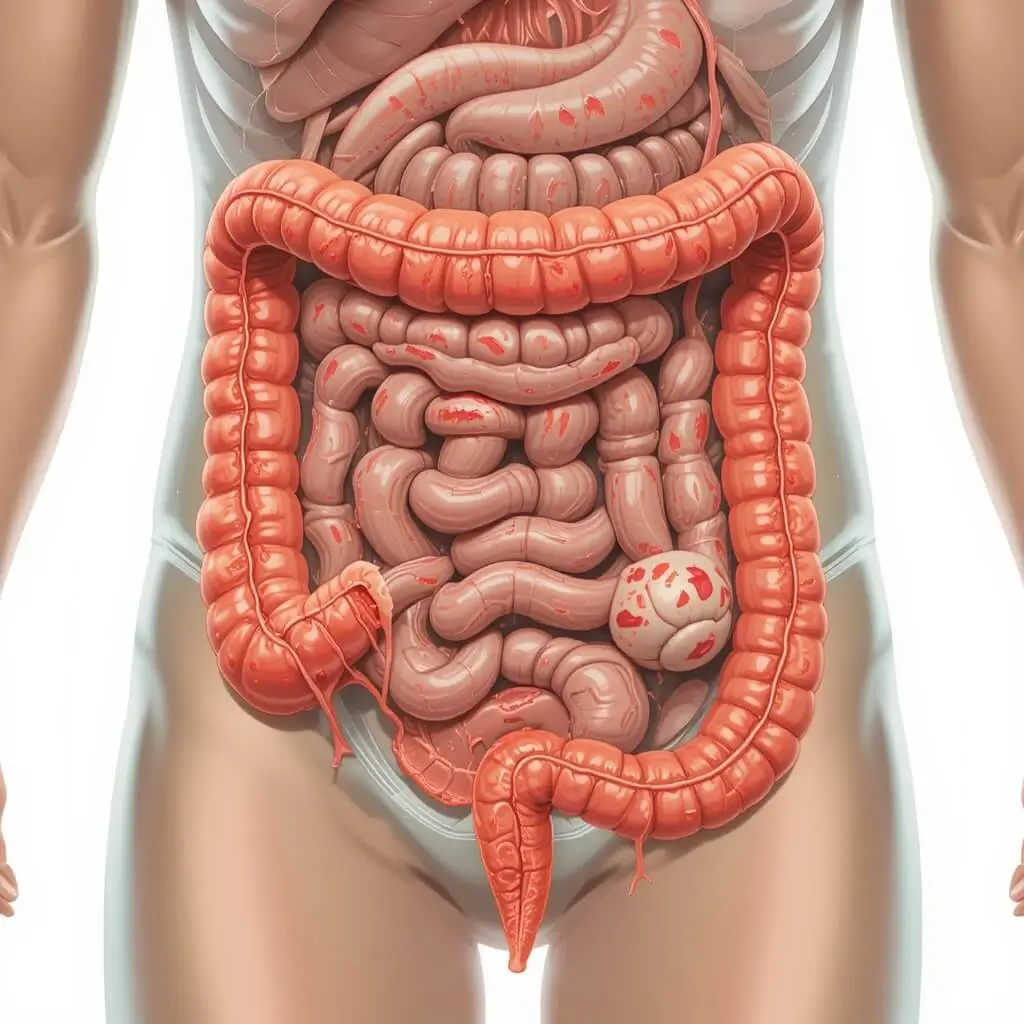
Obesity and Belly Fat – Increased Pressure on the Stomach and Its Link to GERD
Excess weight, particularly abdominal fat, is a well-known risk factor for heartburn, acid reflux, and Gastroesophageal Reflux Disease (GERD). Carrying extra weight around the midsection increases pressure on the stomach, making it more likely for stomach acid to be pushed back into the esophagus.
1. How Obesity Contributes to Acid Reflux
Obesity affects acid reflux in several ways:
- Increased abdominal pressure – Extra belly fat compresses the stomach, forcing acid up into the esophagus.
- Weakened lower esophageal sphincter (LES) – Excess weight, particularly around the abdomen, can cause the LES to relax or malfunction, making it easier for acid to escape.
- Slower digestion and delayed stomach emptying – Obesity is linked to slower gastric emptying, meaning food stays in the stomach longer, increasing acid production and reflux risk.
- Higher inflammation levels – Excess fat tissue produces inflammatory chemicals that can worsen GERD symptoms and esophageal irritation.
2. Belly Fat and Its Direct Impact on GERD
While obesity in general is a risk factor for GERD, central obesity (belly fat) poses the greatest risk because of its direct pressure on the digestive organs.
- More intra-abdominal pressure – Belly fat increases internal pressure, which pushes stomach acid up through the LES.
- Hormonal effects – Fat tissue produces certain hormones that can interfere with digestion and acid regulation.
- Greater risk of hiatal hernia – Obesity increases the risk of hiatal hernia, a condition where part of the stomach pushes through the diaphragm, making acid reflux more severe.
3. How Weight Loss Can Reduce Heartburn and GERD Symptoms
Losing weight, especially around the abdomen, can significantly improve acid reflux symptoms by relieving pressure on the stomach and improving LES function. Studies have shown that even a 5-10% reduction in body weight can lead to noticeable relief from GERD symptoms.
Tips for Managing Weight to Reduce Heartburn:
- Eat smaller, frequent meals – Large meals increase stomach pressure and reflux risk.
- Avoid high-fat, fried foods – These slow digestion and contribute to weight gain.
- Increase fiber intake – Whole grains, vegetables, and fruits help with digestion and weight management.
- Stay physically active – Regular exercise helps maintain a healthy weight and improves digestion.
- Limit late-night eating – Eating too close to bedtime can worsen acid reflux.
By maintaining a healthy weight and reducing belly fat, you can lower the risk of acid reflux and GERD, improving both digestive health and overall well-being.
Stress and Anxiety – Their Effect on Digestion and Stomach Acid Levels
Stress and anxiety have a significant impact on digestive health, particularly in triggering or exacerbating heartburn and acid reflux. These emotional and psychological states can alter how your body produces stomach acid, how efficiently your digestive system works, and how your lower esophageal sphincter (LES) functions.
1. How Stress Affects Stomach Acid Production
When you’re stressed, your body enters the “fight or flight” response, which is a physiological reaction that prepares you to deal with perceived threats. During this response, several changes occur that can negatively impact digestion:
- Increased stomach acid production – Stress and anxiety stimulate the sympathetic nervous system, which can lead to higher stomach acid levels. This excess acid increases the likelihood of it flowing back into the esophagus, causing heartburn.
- Altered digestive enzyme function – Stress can affect the secretion of digestive enzymes, slowing down digestion and leading to the accumulation of food and acid in the stomach.
- Delayed gastric emptying – Stress can slow the movement of food from the stomach into the small intestine, prolonging digestion and increasing the risk of acid reflux.
2. Stress and the Lower Esophageal Sphincter (LES)
The LES is the muscle that acts as a valve between the stomach and the esophagus, preventing stomach acid from flowing upward. However, stress can interfere with the LES’s ability to function properly:
- LES relaxation – High levels of stress and anxiety can cause the LES to relax abnormally, allowing stomach acid to rise into the esophagus.
- Increased sensitivity to reflux – Chronic stress can make the esophagus more sensitive to stomach acid, making heartburn and reflux more painful and frequent.
3. Anxiety and Behavioral Triggers of Acid Reflux
In addition to the physiological effects of stress, anxiety often leads to behaviors that increase the likelihood of heartburn:
- Overeating – When people are stressed or anxious, they may eat more than usual, leading to overloading the stomach and increased pressure on the LES.
- Unhealthy food choices – Stress can lead to cravings for high-fat, spicy, or acidic foods, all of which can trigger heartburn.
- Irregular eating habits – Skipping meals or eating too quickly due to stress can cause digestive problems and exacerbate reflux.
4. How to Manage Stress to Prevent Heartburn
Managing stress and anxiety is key to reducing their impact on heartburn and digestion. Here are some effective strategies to consider:
- Practice relaxation techniques – Yoga, meditation, deep breathing, and mindfulness can all help reduce stress and prevent its negative effects on digestion.
- Exercise regularly – Physical activity reduces stress hormones, improves digestion, and helps maintain a healthy weight, which can also reduce the risk of acid reflux.
- Eat mindfully – Taking the time to chew food slowly and avoid overeating can reduce stomach pressure and improve digestion.
- Avoid triggering foods when stressed – Stay away from fatty, spicy, or acidic foods that are common cravings during stressful times.
- Establish regular meal times – Eating at consistent times and avoiding large meals or snacks late at night can help maintain healthy digestion and prevent acid reflux.
By managing stress effectively and being mindful of its impact on your digestive system, you can reduce the frequency of heartburn and improve overall digestive health.
Best Ways to Prevent Heartburn
Eat Smaller, Balanced Meals – Portion Control and Slow Eating
The size and timing of your meals can have a direct impact on your digestion and the likelihood of experiencing heartburn or acid reflux. Eating smaller, balanced meals and practicing slow eating can help reduce the strain on your digestive system, decrease the production of excess stomach acid, and prevent pressure buildup in the stomach.
1. Why Smaller Meals Help Prevent Heartburn
When you consume large meals, your stomach has to work harder to break down the food, leading to increased stomach acid production. This increased acid production can overwhelm the lower esophageal sphincter (LES), the muscle that prevents acid from flowing back into the esophagus. Larger meals also create more pressure inside the stomach, which can cause acid to leak into the esophagus, resulting in heartburn.
Benefits of smaller meals:
- Reduced stomach pressure – Smaller portions put less strain on the stomach and LES, reducing the risk of acid reflux.
- Easier digestion – The stomach can more easily digest smaller meals, leading to faster emptying and less chance of acid buildup.
- Stable blood sugar levels – Smaller meals throughout the day help maintain more consistent blood sugar levels, preventing large fluctuations that could exacerbate reflux symptoms.
2. Portion Control and Heartburn Prevention
Overeating is a major contributor to heartburn. Consuming large portions of food can cause the stomach to expand too much, which increases internal pressure and can force stomach acid into the esophagus. Portion control is essential in managing heartburn and acid reflux.
Tips for portion control:
- Use smaller plates or bowls – This helps trick your brain into feeling satisfied with smaller portions.
- Pre-portion snacks – Instead of eating straight from a package, pre-portion your snacks to prevent overeating.
- Listen to your body – Eat until you’re satisfied, not full. This helps avoid overeating and excessive stomach pressure.
- Avoid late-night overeating – Eating large meals before bed increases the risk of acid reflux, as it’s harder for food to digest while lying down.
3. The Benefits of Eating Slowly
Eating too quickly is another habit that can contribute to heartburn. When you rush through meals, you’re likely to swallow air, which can cause bloating and increased pressure in the stomach. Additionally, eating quickly leads to overeating because your body doesn’t have enough time to signal when you’re full. Eating slowly allows your digestive system to work more efficiently, reducing the chance of acid reflux.
Benefits of eating slowly:
- Improved digestion – Taking your time to chew food thoroughly helps break it down more easily, allowing the stomach to digest it more effectively.
- Increased satiety – Eating slowly gives your brain enough time to signal that you’re full, helping you avoid overeating.
- Reduced air swallowing – Eating slowly can help minimize the amount of air you swallow, reducing bloating and pressure on the stomach.
4. How to Practice Slow Eating and Portion Control
If you’re looking to eat more slowly and in smaller portions, here are some strategies to help:
- Chew food thoroughly – Take your time to chew each bite at least 20-30 times before swallowing. This will aid digestion and reduce the chances of overeating.
- Put your utensils down between bites – This slows you down and gives your body time to process each bite.
- Focus on your meal – Avoid distractions like TV or smartphones during meals so you can focus on the eating experience and notice when you’re full.
- Set aside time for meals – Create a calm, peaceful environment for meals, allowing yourself to eat without rushing.
- Practice mindful eating – Be aware of how the food makes you feel, both in terms of taste and fullness, to avoid eating past the point of satisfaction.
By adopting the habit of eating smaller, balanced meals and slowing down your eating pace, you can reduce the likelihood of experiencing heartburn and acid reflux. This simple change can make a big difference in your digestive health and overall well-being.
Avoid Trigger Foods and Drinks – Maintaining a GERD-Friendly Diet
For individuals with Gastroesophageal Reflux Disease (GERD) or acid reflux, certain foods and drinks can exacerbate symptoms by relaxing the lower esophageal sphincter (LES) or increasing stomach acid production. Maintaining a GERD-friendly diet involves avoiding common trigger foods and drinks that can worsen heartburn and acid reflux.
1. Common GERD Trigger Foods and Why They Cause Problems
Certain foods and beverages are known to relax the LES, increase acid production, or irritate the esophagus, all of which can trigger or worsen GERD symptoms. Understanding which foods to avoid is essential for managing heartburn and preventing frequent acid reflux episodes.
Trigger foods and drinks include:
- Spicy foods – Spices like chili peppers and hot sauces can irritate the lining of the esophagus and increase stomach acid production, worsening heartburn.
- Tomatoes and citrus fruits – These foods are naturally acidic and can increase acid production in the stomach, making reflux symptoms worse. Common culprits include tomato sauce, citrus juices, and citrus fruits (e.g., oranges, lemons, grapefruits).
- Fatty and fried foods – High-fat foods, such as fried chicken, French fries, or fatty cuts of meat, slow down digestion and increase stomach acid production. They can also relax the LES, allowing acid to flow back into the esophagus.
- Chocolate – Contains caffeine, theobromine, and fat, all of which can relax the LES and lead to acid reflux.
- Garlic and onions – These can irritate the digestive tract and worsen reflux, particularly when consumed in large quantities.
- Caffeine and carbonated beverages – Coffee, tea, soda, and energy drinks contain caffeine, which relaxes the LES, making it easier for stomach acid to rise into the esophagus. Carbonated drinks can also increase bloating and pressure in the stomach, leading to reflux.
- Alcohol – Alcohol, particularly wine, beer, and spirits, can relax the LES and stimulate excess stomach acid production, increasing the risk of heartburn and GERD symptoms.
2. Why Certain Foods Worsen GERD Symptoms
The primary mechanism behind food triggers for GERD is their ability to weaken the LES or increase stomach acid production. The LES is a valve that separates the stomach from the esophagus, and when it is weakened or relaxed, it allows stomach acid to move upwards, causing heartburn. Foods that are fatty, spicy, or acidic can either relax the LES, increase acid production, or irritate the esophagus, all of which make GERD symptoms more likely.
The ways trigger foods affect GERD include:
- Relaxing the LES – Certain foods and beverages, such as chocolate, alcohol, and caffeine, can cause the LES to relax, allowing acid to flow into the esophagus.
- Increasing stomach acid production – Foods like spicy dishes, garlic, citrus, and fried foods can stimulate the stomach to produce more acid, raising the risk of reflux.
- Irritating the esophagus – Acidic foods like tomatoes and citrus fruits can irritate the lining of the esophagus, exacerbating the discomfort caused by acid reflux.
3. GERD-Friendly Foods to Include in Your Diet
While there are many trigger foods to avoid, there are also GERD-friendly foods that are less likely to cause reflux and can help soothe the digestive system. These foods help maintain a healthy balance of stomach acid, improve digestion, and prevent heartburn.
GERD-friendly foods include:
- Non-citrus fruits – Bananas, melons, apples, and pears are gentle on the stomach and help neutralize acid.
- Vegetables – Most vegetables are low in fat and acidity, making them ideal for a GERD-friendly diet. Choose vegetables like broccoli, leafy greens, carrots, and zucchini.
- Lean proteins – Skinless poultry, fish, and plant-based proteins (like tofu and lentils) are great choices that won’t increase stomach acid production.
- Whole grains – Oats, brown rice, quinoa, and whole wheat bread are good sources of fiber that help with digestion and reduce reflux.
- Healthy fats – Opt for monounsaturated fats, such as olive oil, avocados, and nuts, which are less likely to trigger acid reflux compared to fried or fatty foods.
- Ginger – Known for its anti-inflammatory properties, ginger can help reduce nausea and soothe the digestive system. Adding ginger to your meals or drinking ginger tea can be helpful for managing GERD.
4. How to Maintain a GERD-Friendly Diet
To reduce the risk of acid reflux and manage GERD effectively, it’s important to be mindful of your dietary choices. Here are some practical tips for maintaining a GERD-friendly diet:
- Keep a food diary – Track your meals and symptoms to identify which foods trigger your acid reflux, and avoid them.
- Eat smaller, balanced meals – Eating smaller portions helps prevent overloading the stomach, reducing the risk of reflux.
- Avoid eating late at night – Try to eat your last meal 2-3 hours before going to bed to give your stomach time to empty.
- Cook meals at home – Preparing meals at home gives you more control over ingredients and portion sizes, reducing the likelihood of eating trigger foods.
- Choose alkaline snacks – When you need a snack, opt for foods like oatmeal, non-citrus fruits, and whole grain crackers that are less likely to irritate the stomach.
By avoiding trigger foods and choosing GERD-friendly alternatives, you can significantly reduce the frequency and intensity of heartburn, helping you to maintain better digestive health and prevent uncomfortable acid reflux symptoms.
Stay Upright After Meals – The Importance of Posture in Digestion
Maintaining an upright posture after eating plays a crucial role in digestion and can significantly reduce the risk of acid reflux and heartburn. The position of your body after a meal influences how well food moves through your digestive system and how likely it is that stomach acid will backflow into the esophagus.
1. How Posture Affects Digestion
The digestive process is heavily influenced by the position of your body, especially after eating. When you lie down or slouch, the natural process of digestion can be disrupted, leading to discomfort and an increased likelihood of acid reflux. Here’s why staying upright matters:
- Gravity helps food and acid move downward – When you sit or stand upright, gravity helps move food through your digestive tract and encourages the stomach to empty efficiently. This makes it less likely that stomach acid will rise up into the esophagus, which causes heartburn.
- Preventing pressure on the stomach – Posture plays a vital role in reducing pressure on the stomach. Slouching or reclining puts additional pressure on the stomach, which can cause stomach contents, including acid, to move upwards and trigger reflux.
- Reducing bloating and discomfort – Staying upright helps reduce bloating and allows your body to process food without it sitting too long in the stomach, thus preventing unnecessary acid buildup.
2. Lying Down After Eating and Its Impact on Acid Reflux
One of the most significant causes of heartburn and acid reflux is the act of lying down soon after eating. This position makes it easier for stomach acid to travel back into the esophagus, especially if the lower esophageal sphincter (LES) is weak or relaxed. The LES acts as a barrier to prevent acid from rising, but lying flat can disrupt its function.
Why lying down worsens acid reflux:
- Gravity is no longer helping – Without the force of gravity, stomach acid can easily flow back into the esophagus.
- Increased stomach pressure – Lying down causes the stomach to compress, increasing internal pressure, which can force stomach acid up.
- Delayed gastric emptying – Lying down can slow down the process of digestion, allowing food and acid to stay in the stomach longer, increasing the chances of reflux.
3. The Best Posture for Digestion
To reduce the risk of heartburn and promote better digestion, it’s important to practice good posture and remain in an upright position after meals. Here are some tips for optimal posture and positioning:
- Sit upright after meals – Ideally, sit in a chair with your back straight and your shoulders relaxed. This posture allows the food to move through the stomach and intestines more efficiently.
- Stand or take a light walk – After eating, it can be beneficial to go for a short, gentle walk. This helps stimulate digestion and can reduce bloating, gas, and discomfort.
- Avoid lying down – Try to stay upright for at least 2-3 hours after eating to give your body time to digest the food. Lying down too soon increases the likelihood of acid reflux.
- Sit up straight when eating – While eating, ensure that your posture is straight, avoiding slouching or leaning forward. This ensures that your stomach and esophagus are in the best alignment for efficient digestion.
4. How to Maintain Upright Posture for Better Digestion
Adopting and maintaining good posture after meals may take some practice, but the following strategies can help:
- Set reminders to stay upright – If you’re used to lying down or reclining after meals, set a reminder to stay upright for a couple of hours post-meal.
- Use pillows to help elevate your head when resting – If you feel the need to rest, use pillows to elevate your upper body. This can prevent stomach acid from rising into the esophagus, especially during sleep.
- Take short walks after meals – Taking a slow, 10-15 minute walk can assist digestion and encourage the food to move smoothly through your digestive system.
- Avoid heavy meals before bedtime – Try to finish eating at least 2-3 hours before lying down for sleep. Eating large meals late at night increases the chances of reflux while lying down.
By staying upright after meals and practicing good posture, you give your body the best chance to digest food efficiently, avoid acid reflux, and maintain overall digestive health. It’s a simple yet effective habit that can help reduce the discomfort of heartburn and support long-term wellness.
Drink More Water and Herbal Teas – Alkaline Beverages that Neutralize Stomach Acid
Staying hydrated is essential for overall health, and when it comes to managing heartburn and acid reflux, drinking the right fluids can play a significant role. Water and herbal teas are both excellent choices for people with Gastroesophageal Reflux Disease (GERD) or occasional heartburn because they help neutralize stomach acid, promote healthy digestion, and soothe the esophagus.
1. The Importance of Water for Digestion and Acid Neutralization
Water is a fundamental part of your digestive system, and staying well-hydrated can help manage acid reflux in several key ways:
- Neutralizing stomach acid – Drinking water dilutes stomach acid, which can reduce its strength and lessen its ability to irritate the esophagus. By neutralizing stomach acid, water helps to prevent heartburn and discomfort.
- Promoting digestion – Water aids in the overall process of digestion by helping to break down food and ensuring that nutrients are absorbed properly. This reduces the likelihood of acid buildup in the stomach.
- Maintaining healthy mucous production – Staying hydrated ensures that the mucous lining in your stomach and esophagus remains thick and protective, reducing irritation from stomach acid.
- Helping with food movement – Drinking water during meals can also help food move smoothly through your digestive system, preventing the feeling of heaviness or bloating that can lead to acid reflux.
Tip for drinking water: Try drinking room temperature water instead of very cold water, as cold liquids can sometimes exacerbate reflux by causing the stomach to contract.
2. Herbal Teas and Their Role in Neutralizing Stomach Acid
Certain herbal teas have natural properties that can soothe the digestive system and neutralize stomach acid, making them great options for reducing GERD symptoms and heartburn. Many herbal teas have been used for centuries as natural remedies for digestive discomfort, and their calming effects can help prevent acid reflux.
Benefits of herbal teas for heartburn relief:
- Ginger tea – Ginger is a natural anti-inflammatory and has been shown to help reduce nausea and improve digestion. It can soothe the stomach and esophagus, preventing acid from rising into the esophagus and reducing the likelihood of heartburn.
- Chamomile tea – Chamomile has mild sedative properties that help reduce stress and anxiety, which can contribute to acid reflux. It also has anti-inflammatory effects that help calm the digestive tract and reduce irritation caused by stomach acid.
- Licorice tea – Licorice can help protect the lining of the stomach and esophagus from the irritating effects of stomach acid. It also promotes the production of mucus in the digestive system, which helps to protect the esophagus from acid damage.
- Peppermint tea – While peppermint can relax the muscles in the digestive tract and help with bloating, it can trigger acid reflux in some people by relaxing the LES. Therefore, peppermint may not be suitable for everyone with GERD, but it can be helpful for those whose reflux is not aggravated by it.
- Slippery elm tea – Slippery elm forms a gel-like substance when mixed with water, which can coat and soothe the lining of the esophagus, reducing the irritation caused by stomach acid.
3. How Water and Herbal Teas Help Calm Acid Reflux Symptoms
Water and herbal teas provide more than just hydration—they play a role in relieving symptoms and supporting digestion by:
- Soothing the esophagus – Herbal teas and water can help to calm the esophagus if it has become irritated by stomach acid. They can provide a protective coating that reduces the sensation of heartburn.
- Regulating stomach acid levels – By drinking fluids, you can help balance the acidity in your stomach, preventing the overproduction of acid that leads to heartburn.
- Encouraging healthy digestion – Both water and herbal teas help with food breakdown and absorption, reducing the chances of food sitting in the stomach for too long and causing reflux.
4. The Best Times to Drink Water and Herbal Teas
To maximize the benefits of water and herbal teas for acid reflux, consider when and how you drink them:
- Sip water throughout the day – Keep a water bottle handy and sip throughout the day to stay hydrated and prevent acid buildup. Avoid drinking large amounts at once, as this can put extra pressure on your stomach.
- Drink a glass of water before meals – Drinking a glass of water before meals can help dilute stomach acid and prepare your digestive system for food.
- Herbal tea after meals – Drinking herbal teas, such as ginger or chamomile tea, after meals can help calm the digestive system and prevent acid reflux. Avoid drinking teas that are too hot, as they can irritate the esophagus.
- Drink water during meals – Drinking small amounts of water during meals can help with the digestion process, but be mindful not to drink too much, as it may dilute stomach acid and impair digestion.
5. How Much Water and Tea Should You Drink?
While water and herbal teas can help alleviate acid reflux, it’s important not to overdo it. Consuming too much liquid, particularly right before or during a meal, can add pressure to the stomach and lead to reflux.
Guideline for hydration:
- Aim to drink 8-10 cups of water a day, spread out evenly throughout the day, to ensure you stay hydrated.
- When drinking herbal tea, one to two cups after meals are generally enough to soothe the digestive system without overloading it.
By incorporating more water and beneficial herbal teas into your daily routine, you can support digestion, neutralize excess stomach acid, and reduce the discomfort caused by acid reflux and heartburn. This simple dietary adjustment can make a significant difference in managing GERD symptoms and improving your overall digestive health.
Natural Remedies and Medications for Relief
Antacids and H2 Blockers – Over-the-Counter Medications for Quick Relief
When managing heartburn or acid reflux, over-the-counter (OTC) medications like antacids and H2 blockers are commonly used for quick relief. These medications help neutralize excess stomach acid or reduce acid production, providing temporary relief from discomfort. However, it’s important to understand how each type of medication works and when to use them to manage symptoms effectively.
1. What Are Antacids and How Do They Work?
Antacids are one of the most widely used treatments for heartburn and acid reflux. They work by neutralizing stomach acid, which can help alleviate the burning sensation associated with acid reflux. By increasing the pH level in the stomach, antacids help to quickly reduce the acidity, soothing the esophagus and stomach lining.
Common ingredients in antacids include:
- Calcium carbonate (e.g., Tums, Rolaids) – A fast-acting option that neutralizes stomach acid quickly.
- Magnesium hydroxide (e.g., Milk of Magnesia) – Works to neutralize stomach acid and also has a mild laxative effect.
- Aluminum hydroxide (e.g., Maalox, Mylanta) – Commonly combined with magnesium to reduce acidity while also preventing constipation.
- Sodium bicarbonate (e.g., Alka-Seltzer) – Acts quickly to neutralize acid but may cause bloating or gas in some individuals due to the release of carbon dioxide.
Benefits of antacids:
- Fast relief – Antacids can relieve heartburn and indigestion within minutes by neutralizing acid.
- Effective for mild acid reflux – They work well for occasional heartburn or mild acid reflux, offering temporary relief.
- Convenience – Available in chewable tablets, liquid form, and effervescent tablets, making them easy to take and use on the go.
Limitations of antacids:
- Short-lasting relief – While effective for quick relief, the effects of antacids are usually temporary, and they may need to be taken more frequently.
- Not suitable for chronic reflux – For frequent or severe GERD, antacids alone may not be enough to manage symptoms long-term.
2. What Are H2 Blockers and How Do They Work?
H2 blockers (also known as histamine-2 receptor antagonists) are another type of OTC medication that reduces stomach acid production. Unlike antacids, which neutralize existing acid, H2 blockers work by blocking the action of histamine, a substance that stimulates acid production in the stomach. This results in reduced acid secretion, helping to alleviate heartburn and acid reflux symptoms.
Common H2 blockers include:
- Ranitidine (e.g., Zantac) – One of the most widely known H2 blockers, although its availability may vary due to safety concerns in some regions.
- Famotidine (e.g., Pepcid) – Another common H2 blocker that is available in both prescription and over-the-counter formulations.
- Cimetidine (e.g., Tagamet) – Often used for the treatment of ulcers and acid reflux, but can have drug interactions.
- Nizatidine (e.g., Axid) – Another option for reducing stomach acid production.
Benefits of H2 blockers:
- Longer-lasting relief than antacids – H2 blockers take longer to work than antacids but provide longer-lasting relief, typically lasting up to 12 hours.
- Effective for mild to moderate acid reflux – They are often recommended for people who experience frequent heartburn or mild GERD.
- Preventative use – H2 blockers can be taken before meals to prevent heartburn or acid reflux, especially if certain foods tend to trigger symptoms.
Limitations of H2 blockers:
- Slower onset of relief – Unlike antacids, H2 blockers take longer to work, typically 30-60 minutes, and may not provide instant relief.
- Not effective for severe acid reflux – H2 blockers are generally effective for mild to moderate GERD but may not be strong enough for more severe cases.
3. When to Use Antacids vs. H2 Blockers
The choice between antacids and H2 blockers depends on the severity of your symptoms and how often they occur:
- For quick, short-term relief: If you need immediate relief from occasional heartburn or indigestion, antacids are often the better choice because they act quickly.
- For longer-lasting relief: If you experience frequent heartburn or mild acid reflux throughout the day, H2 blockers may be more effective because they provide longer-lasting relief and reduce the overall acid production in your stomach.
- For prevention: H2 blockers can be taken before meals to prevent heartburn or acid reflux, especially if you know certain foods or situations trigger symptoms.
- For persistent or severe GERD: If you have chronic acid reflux or severe GERD, you may need a combination of medications or a stronger prescription medication. In these cases, consulting with a healthcare provider is essential.
4. Potential Side Effects and Precautions
While antacids and H2 blockers are generally safe when used as directed, they can have side effects or interactions with other medications:
Antacids side effects and precautions:
- Constipation or diarrhea – Depending on the type of antacid, you may experience constipation (with aluminum-based antacids) or diarrhea (with magnesium-based antacids).
- Electrolyte imbalances – Long-term or excessive use of antacids can lead to low calcium or magnesium levels, especially with high doses of calcium carbonate or magnesium.
- Drug interactions – Antacids can interfere with the absorption of other medications, so it’s important to check with your healthcare provider if you’re taking other medications.
H2 blockers side effects and precautions:
- Headaches or dizziness – Common side effects include headaches, dizziness, or nausea, especially with higher doses.
- Potential drug interactions – H2 blockers can interact with certain medications, such as warfarin or other drugs metabolized by the liver, so it’s important to consult with a healthcare provider if you’re on other medications.
- Tolerance – Over time, the effectiveness of H2 blockers may decrease as your body becomes tolerant, requiring a higher dose for the same effect.
5. When to Seek Professional Help
While antacids and H2 blockers can be effective for managing occasional heartburn or mild acid reflux, it’s essential to seek medical advice if:
- Your symptoms become frequent or severe, suggesting chronic GERD.
- You experience difficulty swallowing, unexplained weight loss, or persistent chest pain, which could indicate a more serious condition.
- Over-the-counter medications don’t provide adequate relief or if you find yourself relying on them frequently.
In these cases, a healthcare professional may recommend stronger prescription medications or other treatments to address the root cause of your symptoms.
Conclusion:
Antacids and H2 blockers are helpful over-the-counter treatments for managing heartburn and acid reflux. While antacids provide quick, short-term relief by neutralizing stomach acid, H2 blockers reduce acid production for longer-lasting relief. Choosing the right medication depends on your specific symptoms and the frequency of acid reflux, but they are most effective when used appropriately and in combination with lifestyle changes for long-term management of acid reflux and GERD.
Proton Pump Inhibitors (PPIs) – Long-Term Medication Options for Chronic Cases

Proton Pump Inhibitors (PPIs) are a class of medications commonly used to treat chronic acid reflux and Gastroesophageal Reflux Disease (GERD). Unlike antacids and H2 blockers, which provide temporary relief by neutralizing or reducing stomach acid, PPIs work by blocking the proton pump in the stomach, which is responsible for producing stomach acid. By inhibiting this pump, PPIs significantly reduce the overall amount of acid produced in the stomach, providing long-term relief for people suffering from severe or persistent acid reflux.
1. How PPIs Work and Why They Are Effective
The proton pump is a mechanism located in the stomach lining that produces hydrochloric acid, a key component of stomach acid. When the proton pump is blocked by a PPI, acid production is greatly reduced, giving the esophagus and stomach time to heal and reducing the likelihood of heartburn and other symptoms of GERD.
- Blocking acid production: PPIs inhibit the final step in acid secretion by the stomach’s proton pump, leading to a dramatic reduction in acid levels. This makes PPIs particularly effective for those with severe GERD, ulcers, or damage to the esophagus (e.g., esophagitis).
- Healing the esophagus: The reduction in stomach acid provides time for the esophagus to heal, especially in cases where the lining has been damaged due to chronic acid reflux. This healing is important in preventing more serious complications like Barrett’s esophagus or esophageal cancer.
2. Common PPIs and How They Work
PPIs are available in both prescription and over-the-counter forms. Some common brand names and generic versions of PPIs include:
- Omeprazole (e.g., Prilosec)
- Lansoprazole (e.g., Prevacid)
- Esomeprazole (e.g., Nexium)
- Pantoprazole (e.g., Protonix)
- Rabeprazole (e.g., AcipHex)
- Dexlansoprazole (e.g., Dexilant)
PPIs come in pill, capsule, and liquid forms, with delayed-release formulations designed to act over a prolonged period, allowing for better control of acid production throughout the day.
3. Benefits of PPIs for Chronic GERD and Heartburn
PPIs are the preferred treatment for chronic or severe acid reflux, and they offer several benefits for managing long-term symptoms:
- Effective for severe acid reflux: PPIs are highly effective at reducing stomach acid production, making them ideal for those who have not found relief with antacids or H2 blockers.
- Healing of esophageal damage: For individuals with erosive esophagitis or Barrett’s esophagus (conditions caused by chronic acid reflux), PPIs can help heal the esophagus by reducing the acidic environment that causes inflammation and irritation.
- Long-term relief: Unlike antacids or H2 blockers, which work in a short time frame, PPIs provide long-lasting relief for individuals suffering from daily or persistent heartburn or GERD symptoms. They can be taken once a day (or as prescribed by a doctor) and provide relief for up to 24 hours.
- Prevention of ulcers: PPIs are commonly used to prevent or treat peptic ulcers (sores in the stomach or duodenum), which can result from chronic acid exposure. They also help in preventing ulcers caused by NSAID (nonsteroidal anti-inflammatory drug) use, as they lower stomach acid levels.
4. Long-Term Use and Potential Risks of PPIs
While PPIs are highly effective for managing chronic GERD and other acid-related conditions, long-term use can come with potential risks and side effects. It’s important for people to use PPIs under the supervision of a healthcare provider and for the prescribed duration to minimize risks.
Potential risks of long-term PPI use:
- Nutrient deficiencies: Chronic use of PPIs can interfere with the absorption of certain nutrients, such as calcium, magnesium, iron, and vitamin B12. This can lead to deficiencies that may require supplementation.
- Increased risk of fractures: The reduction in stomach acid can interfere with calcium absorption, which increases the risk of bone fractures, particularly in older adults.
- Kidney disease: There is some evidence suggesting that long-term use of PPIs may be associated with an increased risk of kidney disease or kidney damage. This is especially true for those who have other risk factors like pre-existing kidney conditions.
- Infections: Stomach acid acts as a natural barrier against pathogens. Long-term PPI use can increase the risk of infections, particularly Clostridium difficile (C. diff) infections in the intestines, and pneumonia.
- Rebound acid hypersecretion: Discontinuing PPIs abruptly may cause a rebound effect, where the stomach temporarily produces more acid than before, worsening acid reflux symptoms. This is why PPIs should be tapered down under a doctor’s guidance if they are being stopped.
5. When to Use PPIs and How to Use Them
PPIs are generally recommended for people with chronic acid reflux or severe GERD. They can also be prescribed for other conditions like gastric ulcers and ** Zollinger-Ellison syndrome** (a condition involving excessive stomach acid production).
Guidelines for PPI use:
- Short-term use for acute conditions: For conditions like ulcers or severe esophagitis, PPIs may be prescribed for a few weeks to heal the stomach lining and reduce acid damage.
- Long-term use for chronic GERD: If you suffer from chronic GERD, PPIs may be prescribed for long-term use, but typically for a limited duration (6-12 months), followed by periodic re-evaluation of the treatment plan.
- Taking PPIs properly: PPIs are typically taken once daily, in the morning before meals, to provide maximum benefit. It’s important to follow the prescribed dosage and avoid taking PPIs with certain foods or medications that can interfere with absorption.
6. Alternatives to PPIs
While PPIs are highly effective, some people may need alternatives due to side effects or other concerns. These alternatives may include:
- H2 blockers for less severe cases of acid reflux.
- Prokinetic agents that improve gastric motility and reduce acid reflux.
- Surgical interventions such as fundoplication for severe GERD that doesn’t respond to medication.
- Lifestyle changes like weight loss, dietary adjustments, and avoiding trigger foods.
Conclusion
Proton Pump Inhibitors (PPIs) are an essential tool for managing chronic acid reflux and severe GERD, providing long-term relief by significantly reducing stomach acid production. While they are highly effective for treating acid-related conditions and promoting esophageal healing, long-term use requires careful consideration of potential risks, including nutrient deficiencies, bone fractures, and kidney issues. For people with chronic acid reflux, PPIs can offer significant relief, but they should be used under the guidance of a healthcare provider, and lifestyle modifications should also be incorporated to manage symptoms effectively.
Home Remedies: Ginger, Aloe Vera, and Bananas – Natural Ways to Soothe Heartburn
When dealing with heartburn or acid reflux, many people look for natural remedies to provide relief, either as a first line of defense or in addition to other treatments. Ginger, aloe vera, and bananas are three natural options that have been used for centuries to soothe the digestive system and relieve heartburn symptoms. These remedies are gentle on the stomach and can be part of an overall strategy to manage mild to moderate acid reflux. Let’s dive deeper into how each of these natural remedies works to combat heartburn.
1. Ginger – A Natural Anti-inflammatory for Digestive Health
Ginger is well-known for its medicinal properties and has long been used in traditional medicine for its ability to ease digestive discomfort. It can be especially helpful for people who experience heartburn or indigestion because it has natural anti-inflammatory and soothing properties that help calm the stomach.
- How Ginger Helps with Heartburn:
Ginger works by helping to reduce stomach acid production while also promoting better digestion. It can help speed up gastric emptying, which means food and stomach acids move through the digestive system more efficiently. This is particularly important for those who suffer from acid reflux or delayed gastric emptying (when food sits in the stomach for too long, leading to an increased risk of reflux). Ginger also contains gingerols and shogaols, compounds that have been shown to help with inflammation in the digestive tract, reducing the risk of irritation from stomach acid. Additionally, ginger can help relieve nausea, which often accompanies heartburn or acid reflux. - How to Use Ginger for Heartburn:
- Ginger tea: One of the most popular ways to use ginger is by making a soothing ginger tea. You can make this by steeping fresh ginger slices in hot water for 5-10 minutes. You may add honey or lemon for taste.
- Ginger chews or capsules: If you’re looking for a more concentrated form of ginger, you can take ginger supplements (available in chewable form or capsules) after meals to help prevent acid reflux.
- Fresh ginger: Simply chewing on a small piece of fresh ginger root after meals can help with digestion and soothe heartburn.
2. Aloe Vera – Healing and Anti-inflammatory Properties
Aloe vera, known for its healing properties when applied topically, is also beneficial when consumed orally. The gel inside the aloe vera plant contains a wide range of nutrients, including vitamins, minerals, and amino acids that can help soothe and reduce inflammation in the digestive system.
- How Aloe Vera Helps with Heartburn:
Aloe vera has natural anti-inflammatory properties that can help reduce irritation in the esophagus and stomach. It also has a cooling effect, which can soothe the burning sensation associated with heartburn. Aloe vera has been shown to help reduce acid reflux, as it may assist in improving the functioning of the lower esophageal sphincter (LES)—the muscle that prevents stomach acid from flowing back into the esophagus.
Additionally, aloe vera may support the healing of the esophagus in individuals with esophagitis or inflammation caused by chronic acid reflux. - How to Use Aloe Vera for Heartburn:
- Aloe vera juice: Aloe vera juice is widely available in health food stores and is often consumed to soothe heartburn. Make sure to choose organic, pure aloe vera juice, and opt for a product with no added sugars or artificial ingredients. Start with a small amount (around 1/4 cup) before meals, as larger quantities may have a laxative effect.
- Aloe vera gel: You can also try adding pure aloe vera gel to smoothies or juices for digestive benefits. Make sure the gel is food-grade to ensure it’s safe for consumption.
3. Bananas – A Gentle and Alkaline Fruit for Soothing Heartburn
Bananas are a mild, easily digestible fruit that is commonly recommended for individuals suffering from acid reflux or heartburn. They are naturally alkaline, which means they can help neutralize stomach acid and provide a protective barrier to the stomach lining.
- How Bananas Help with Heartburn:
Bananas are rich in potassium, a mineral that helps maintain proper electrolyte balance in the body and aids in digestion. The natural alkaline nature of bananas can help neutralize excess stomach acid and prevent the painful sensation of heartburn. Bananas also contain pectin, a type of soluble fiber that can help soothe the stomach lining and support healthy digestion by promoting smoother bowel movements and preventing constipation.
Because bananas are easy on the stomach and less likely to trigger reflux, they are often included in bland diets designed to reduce irritation in the digestive system. - How to Use Bananas for Heartburn:
- Eat a ripe banana: Simply eating a banana (preferably ripe) after meals can help neutralize stomach acid and prevent heartburn.
- Banana smoothies: For a soothing snack or breakfast, try making a banana smoothie by blending a ripe banana with almond milk or another non-acidic liquid. Adding a handful of spinach or ginger can further boost its anti-inflammatory effects.
Other Considerations and Tips for Using Natural Remedies
- Consistency Is Key: While ginger, aloe vera, and bananas can provide relief, they are generally more effective when used consistently over time, as part of a broader lifestyle plan to manage heartburn.
- Moderation and Dosage: It’s important to use these remedies in moderation. For example, too much aloe vera juice can cause diarrhea, and excessive consumption of ginger may lead to stomach upset or digestive discomfort. Always start with small amounts and monitor how your body reacts.
- Consult a Healthcare Provider: If you have chronic acid reflux or GERD, it’s important to work with your healthcare provider to develop a comprehensive treatment plan. Natural remedies like ginger, aloe vera, and bananas can be effective for mild symptoms, but they should complement medical treatments, especially for more severe cases.
Conclusion
Natural remedies like ginger, aloe vera, and bananas can be effective and soothing options for people looking to manage mild heartburn or acid reflux. These foods and herbs have anti-inflammatory and alkaline properties that help neutralize stomach acid, heal the digestive tract, and provide relief from the burning sensation associated with acid reflux. However, they should be used in conjunction with a balanced diet and lifestyle changes, and it’s always a good idea to consult with a healthcare provider before starting any new remedy, especially if you have chronic symptoms or underlying conditions.
The Role of an Alkaline Diet – How Diet Adjustments Can Reduce Acidity
An alkaline diet is based on the idea of consuming foods that promote a more alkaline (or less acidic) environment in the body, which can help manage various conditions, including heartburn, acid reflux, and GERD (Gastroesophageal Reflux Disease). The theory behind an alkaline diet is that the foods we eat can influence the pH balance in our blood and digestive system. By choosing more alkaline-forming foods, we can potentially reduce excess acidity in the body and soothe the symptoms of heartburn and reflux.
1. Understanding pH and Acidity in the Body
The pH scale ranges from 0 to 14, with 7 being neutral. Values below 7 are considered acidic, while those above 7 are alkaline. The body needs to maintain a slightly alkaline pH in the blood, typically around 7.35 to 7.45, to function optimally. Certain foods can have an alkaline effect when digested, helping to maintain this balance, while others may have an acid-forming effect, increasing the acidity in the body.
- Alkaline-forming foods: These are foods that, after digestion and metabolism, leave an alkaline residue in the body. Examples include fruits, vegetables, almonds, and legumes.
- Acid-forming foods: These foods tend to increase acidity in the body after digestion. Common examples include meat, dairy, sugar, and refined grains.
2. Alkaline Foods and Their Impact on Heartburn and Acid Reflux
By focusing on more alkaline-forming foods, individuals with heartburn or acid reflux can potentially help neutralize excess stomach acid and reduce the frequency and intensity of symptoms. Here’s how certain alkaline foods may play a role in reducing acidity:
- Fruits: Many fruits, especially bananas, apples, melons, and papaya, have a naturally alkaline nature that can help soothe the digestive tract. For example, bananas are often recommended for acid reflux because they are not only alkaline but also high in pectin, a type of soluble fiber that helps with digestion and prevents constipation, which can contribute to reflux.
- Bananas: High in potassium and naturally alkaline, they help neutralize stomach acid and promote digestion.
- Melons: Low in acid, melons like cantaloupe and watermelon can soothe the stomach lining and reduce irritation caused by acid reflux.
- Vegetables: Leafy greens and vegetables like spinach, broccoli, cucumbers, and asparagus are naturally alkaline and are excellent choices for an alkaline diet. They help balance stomach acid levels, provide fiber for digestion, and promote alkalinity in the body. Vegetables are generally easy to digest and provide essential vitamins and minerals without triggering heartburn.
- Spinach: Rich in magnesium, which can help relax the digestive muscles and improve esophageal function.
- Cucumbers: High in water content and soothing on the digestive system, cucumbers can help reduce the effects of heartburn and indigestion.
- Alkaline Waters: Some people also turn to alkaline water—which has a higher pH level than regular tap water—as a way to help neutralize stomach acid and provide hydration. Drinking water with a higher pH can help dilute stomach acid and support digestion.
- Nuts and Seeds: Almonds, chia seeds, and flaxseeds are considered alkaline-forming foods and can be good sources of healthy fats and fiber. Almonds in particular are often recommended for acid reflux, as they are alkaline and rich in magnesium, which can help prevent acid reflux.
3. Reducing Acidic Foods to Prevent Heartburn
In addition to adding more alkaline-forming foods to your diet, reducing the intake of acid-forming foods is another essential aspect of the alkaline diet approach. Certain foods can increase stomach acidity and irritate the lining of the esophagus, making acid reflux and heartburn symptoms worse. Here’s a breakdown of some acid-forming foods that should be minimized or avoided:
- Citrus Fruits: While fruits like oranges, grapefruits, and lemons are rich in vitamin C, their high citric acid content can aggravate acid reflux and heartburn symptoms in some people. While they are acidic before digestion, some may find that the acidic nature persists and worsens symptoms.
- Tomatoes: Like citrus fruits, tomatoes are naturally acidic and can trigger acid reflux, especially in individuals who already have a sensitive digestive system. Foods like tomato sauce, ketchup, and pizza should be consumed in moderation.
- Spicy Foods: Chili peppers, spicy sauces, and foods with strong spices (such as curry or hot sauces) can irritate the digestive tract and relax the lower esophageal sphincter (LES), making acid reflux more likely.
- Processed Foods: Refined grains, sugary snacks, and highly processed junk foods tend to be acid-forming and often lack the nutrients needed to support healthy digestion. These foods can contribute to inflammation and exacerbate heartburn.
- Caffeinated and Carbonated Beverages: Caffeine and carbonated drinks, such as soda, coffee, and energy drinks, can irritate the stomach lining and relax the LES, allowing acid to travel up into the esophagus. Switching to herbal teas or water may be a better choice for individuals with reflux.
4. Additional Benefits of an Alkaline Diet
An alkaline diet not only helps reduce acid reflux and heartburn but also supports overall health in several ways:
- Improved digestion: An alkaline diet can support smoother digestion and help prevent constipation, bloating, and other digestive discomforts that often accompany acid reflux.
- Weight management: Alkaline-forming foods, especially fruits and vegetables, tend to be lower in calories and rich in fiber, which promotes satiety and can help with weight loss. Since obesity is a significant risk factor for acid reflux and GERD, maintaining a healthy weight can reduce the frequency and severity of heartburn.
- Reduced inflammation: Many alkaline foods, particularly leafy greens and fruits, are rich in antioxidants, which help reduce inflammation throughout the body. This can be particularly beneficial for individuals with chronic acid reflux or GERD, as ongoing inflammation in the digestive tract can worsen symptoms.
- Enhanced hydration: Many alkaline-forming foods, such as fruits and vegetables, have high water content. Proper hydration is essential for overall digestive health and can help dilute stomach acid, reducing the intensity of heartburn.
5. Getting Started with an Alkaline Diet for Heartburn Relief
If you’re considering an alkaline diet to help manage your heartburn or acid reflux, here are a few practical tips to get started:
- Start with a variety of fruits and vegetables: Focus on consuming plenty of alkaline-forming foods like leafy greens, apples, pears, and bananas to promote an alkaline environment in your body.
- Hydrate with alkaline water: Try incorporating alkaline water into your routine, especially if you experience frequent heartburn. Drink water throughout the day to help dilute stomach acid.
- Avoid trigger foods: Minimize your intake of acidic or spicy foods like citrus, tomatoes, and fried or processed foods that can exacerbate heartburn.
- Cook with alkaline herbs: Use herbs like ginger, turmeric, and parsley to add flavor to your meals and help reduce inflammation in your digestive tract.
Conclusion
An alkaline diet can be an effective way to help reduce acidity in the body and provide relief from heartburn and acid reflux. By focusing on alkaline-forming foods like fruits, vegetables, nuts, and seeds, and avoiding acid-forming foods such as citrus fruits, tomatoes, and processed snacks, individuals can promote a balanced pH in the digestive system, support healthy digestion, and reduce the frequency and severity of acid reflux symptoms. While an alkaline diet can provide significant benefits, it should be used in conjunction with other lifestyle changes and treatments for optimal heartburn management.
Conclusion: Managing Heartburn Through Lifestyle and Dietary Adjustments
In conclusion, heartburn is a common yet uncomfortable condition that many people experience at some point in their lives. It’s typically triggered by factors such as dietary choices, lifestyle habits, and underlying health conditions like GERD (gastroesophageal reflux disease). Understanding the various triggers and adopting preventative measures can significantly improve the quality of life for those who suffer from frequent heartburn.
The key to managing heartburn lies in a combination of dietary adjustments, lifestyle changes, and, when necessary, medications. Through simple changes such as eating smaller, balanced meals, avoiding trigger foods like spicy and acidic items, and maintaining a proper posture after eating, individuals can reduce the frequency and severity of heartburn episodes.
In addition to lifestyle changes, an alkaline diet—rich in fruits, vegetables, and alkaline water—can help neutralize stomach acids and provide relief from symptoms. Foods like ginger, aloe vera, and bananas offer natural alternatives to pharmaceutical treatments, providing soothing effects for those who seek gentler solutions. For those experiencing more persistent or chronic heartburn, medications such as antacids, H2 blockers, or proton pump inhibitors (PPIs) can be used under the guidance of a healthcare provider to control acidity and provide long-term relief.
It’s important to remember that heartburn and acid reflux are often manageable conditions, and with the right approach, many people can reduce their symptoms or even prevent them altogether. Consulting with a healthcare professional for proper diagnosis and tailored treatment options is recommended, especially if heartburn is persistent or worsens over time.
Ultimately, prevention is key. By recognizing triggers, making healthier food choices, and embracing a holistic approach to health, you can regain control of your digestive well-being and enjoy meals without the discomfort of heartburn. Remember, small and consistent changes to your diet, lifestyle, and stress management can go a long way in improving your digestive health and overall quality of life.