Crohn’s Disease is a chronic inflammatory condition that affects the digestive tract, primarily the small intestine and colon. As a type of Inflammatory Bowel Disease (IBD), it causes persistent inflammation that can lead to severe abdominal pain, diarrhea, weight loss, and fatigue. While the exact cause remains unknown, genetics, immune system dysfunction, and environmental factors are believed to play a role in its development.
Unlike other digestive disorders, Crohn’s Disease is a lifelong condition with no known cure, but with the right treatment and lifestyle adjustments, many individuals can effectively manage their symptoms and lead fulfilling lives. In this comprehensive guide, we will explore its symptoms, causes, diagnosis, treatment options, and strategies for managing flare-ups. Whether you are newly diagnosed or looking to deepen your understanding, this article will provide essential insights into Crohn’s Disease and how to navigate its challenges.
- What is Crohn’s Disease?
- Symptoms and Causes of Crohn’s Disease
- Diagnosing Crohn’s Disease
- Treatment Options for Crohn’s Disease
- Conclusion: Managing Crohn’s Disease
- 📚 Recommended Readings and Expert Advice
What is Crohn’s Disease?
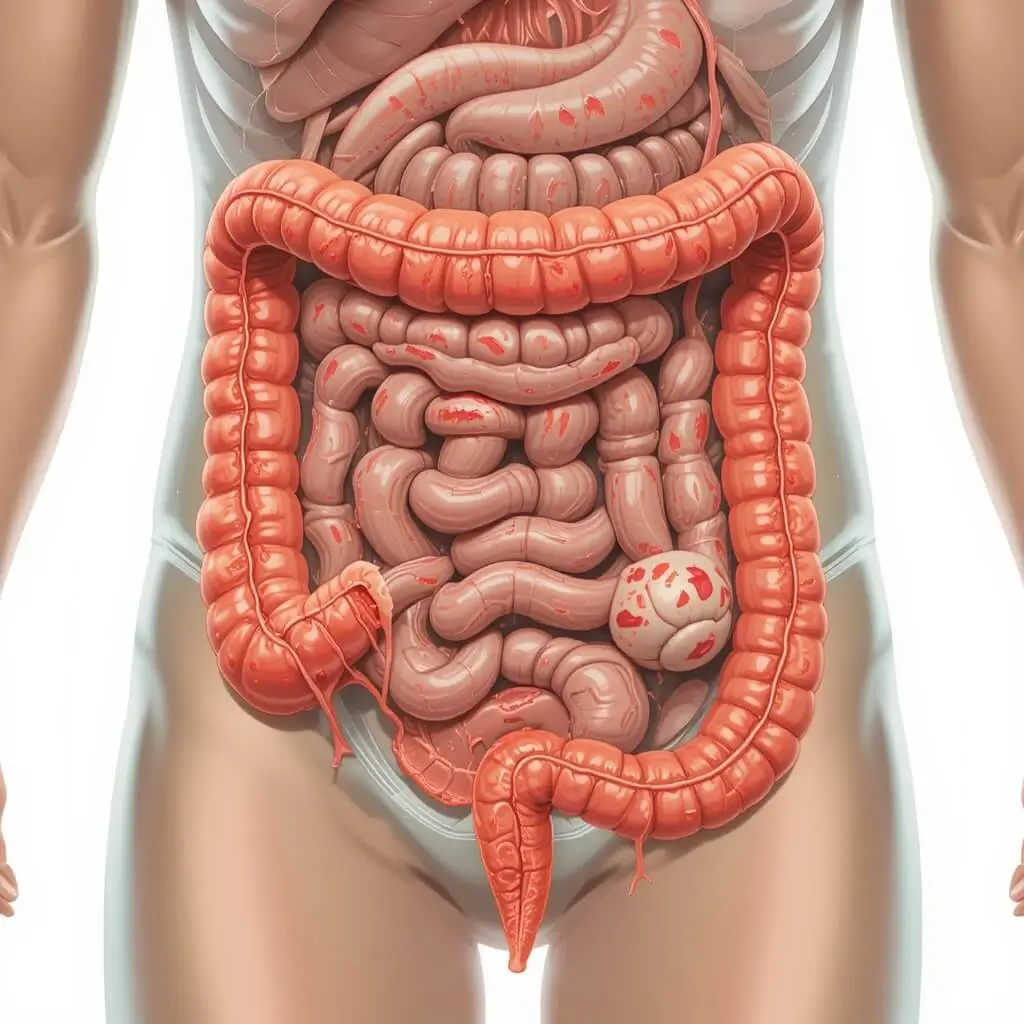
Crohn’s Disease is a chronic inflammatory condition that affects the digestive system, primarily targeting the small intestine and colon. It is a form of Inflammatory Bowel Disease (IBD), a group of disorders that cause long-term inflammation in the gastrointestinal (GI) tract. Unlike ulcerative colitis, which is another type of IBD that only affects the colon and rectum, Crohn’s Disease can impact any part of the digestive tract, from the mouth to the anus.
How Does Crohn’s Disease Affect the Digestive System?
Crohn’s Disease causes inflammation that can penetrate deep into the layers of the intestinal wall. This inflammation can lead to complications such as:
- Ulcers: Open sores in the lining of the intestines.
- Strictures: Narrowing of the intestines due to scar tissue, which can cause blockages.
- Fistulas: Abnormal connections between different parts of the intestine or between the intestine and other organs.
Because the disease can appear anywhere in the digestive tract, its symptoms and severity vary from person to person. Some people experience mild, intermittent symptoms, while others have severe, debilitating flare-ups that require medical intervention.
Is Crohn’s Disease an Autoimmune Condition?
Crohn’s Disease is often classified as an autoimmune or immune-mediated disorder, meaning the immune system mistakenly attacks healthy cells in the digestive tract, leading to chronic inflammation. While the exact cause of this immune response is not fully understood, research suggests that genetics, environmental triggers, and an overactive immune system contribute to its development.
Who is at Risk for Crohn’s Disease?
Crohn’s Disease can affect people of all ages, but it is most commonly diagnosed in:
- Young adults (ages 15-35) – The majority of cases develop in early adulthood.
- Individuals with a family history – Having a close relative with Crohn’s increases the risk.
- People living in Western countries – Higher rates are found in North America and Europe, possibly due to diet and environmental factors.
- Smokers – Studies show that smoking increases the risk and severity of Crohn’s Disease.
Types of Crohn’s Disease
Depending on which part of the digestive tract is affected, Crohn’s Disease is classified into different types:
- Ileocolitis – The most common form, affecting the ileum (last part of the small intestine) and colon.
- Ileitis – Involves only the ileum, leading to pain, diarrhea, and possible complications like fistulas.
- Gastroduodenal Crohn’s Disease – Affects the stomach and the beginning of the small intestine (duodenum).
- Jejunoileitis – Causes inflammation in the middle section of the small intestine (jejunum), leading to cramps and malabsorption.
- Crohn’s Colitis – Limited to the colon, causing severe diarrhea, rectal bleeding, and fistula formation.
Understanding the nature of Crohn’s Disease is essential for early diagnosis and effective management. In the next section, we will explore its symptoms and causes, helping individuals recognize early warning signs and potential risk factors.
Symptoms and Causes of Crohn’s Disease

Crohn’s Disease is a complex condition that affects people differently, with symptoms ranging from mild to severe. Some individuals experience occasional flare-ups, while others suffer from persistent, debilitating symptoms that interfere with daily life. Understanding the symptoms and causes of Crohn’s Disease is crucial for early diagnosis and effective management.
Common Symptoms of Crohn’s Disease
The symptoms of Crohn’s Disease vary depending on the location and severity of inflammation in the digestive tract. While some individuals experience mild discomfort, others may face serious complications requiring medical intervention.
1. Gastrointestinal Symptoms
Since Crohn’s Disease primarily affects the digestive system, the most common symptoms involve the stomach and intestines:
- Chronic diarrhea – Loose, frequent stools due to inflammation and malabsorption.
- Abdominal pain and cramping – Often occurs in the lower right abdomen, especially when the ileum (small intestine) is affected.
- Blood in stool – Caused by ulcers or inflammation in the colon.
- Urgency to defecate – Feeling the frequent need to use the restroom, sometimes without passing stool.
2. Systemic (Whole-Body) Symptoms
Crohn’s Disease is not just a gastrointestinal condition; it also affects overall health, leading to:
- Fatigue – Persistent tiredness due to inflammation and poor nutrient absorption.
- Weight loss and malnutrition – Inability to properly absorb nutrients from food.
- Fever – Common during flare-ups, indicating active inflammation.
3. Extraintestinal (Outside the Gut) Symptoms
Crohn’s Disease can also cause symptoms outside the digestive system, including:
- Joint pain and arthritis – Inflammation in joints, similar to rheumatoid arthritis.
- Skin problems – Red, swollen patches or ulcers, particularly on the legs.
- Eye inflammation – Conditions like uveitis (eye redness and pain).
- Mouth ulcers – Painful sores inside the mouth.
Causes and Risk Factors of Crohn’s Disease
The exact cause of Crohn’s Disease is unknown, but research suggests it is triggered by a combination of genetic, immune, and environmental factors.
1. Genetic Factors: Family History and Hereditary Risk
- Studies indicate that up to 20% of Crohn’s patients have a family history of Inflammatory Bowel Disease (IBD).
- Certain genetic mutations, such as variations in the NOD2 gene, may increase the risk of developing the disease.
2. Immune System Dysfunction: An Autoimmune Response
- Crohn’s Disease is considered an immune-mediated disorder, where the body’s immune system mistakenly attacks healthy cells in the digestive tract, leading to chronic inflammation.
- Some scientists believe the immune system overreacts to bacteria in the gut microbiome, causing excessive inflammation.
3. Environmental Triggers: Lifestyle and External Factors
Several environmental and lifestyle factors have been linked to Crohn’s Disease:
- Diet: High-fat, processed foods and a lack of fiber may contribute to gut inflammation.
- Smoking: Smokers are twice as likely to develop Crohn’s Disease, and symptoms tend to be more severe.
- Stress and Mental Health: While stress does not cause Crohn’s, it can worsen flare-ups.
- Gut Microbiome Imbalance: Disruptions in the balance of good and bad bacteria in the intestines may contribute to Crohn’s Disease.
Who is Most at Risk for Crohn’s Disease?
While Crohn’s Disease can affect anyone, certain groups are at higher risk:
✅ Young adults (ages 15-35) – Most cases are diagnosed in early adulthood.
✅ People with a family history of IBD – A close relative with Crohn’s or ulcerative colitis increases risk.
✅ Residents of Western countries – Higher incidence in the U.S., Canada, and Europe.
✅ Smokers – Higher risk of severe disease progression.
✅ Individuals with a history of antibiotic overuse – Overuse of antibiotics may disrupt gut bacteria, increasing susceptibility.
Early Detection is Key
Recognizing the early signs of Crohn’s Disease can lead to faster diagnosis and treatment, improving long-term health outcomes. If you experience persistent digestive issues, unexplained weight loss, or chronic fatigue, consult a gastroenterologist for a medical evaluation.
In the next section, we’ll explore the diagnosis process and the tests used to confirm Crohn’s Disease.
Diagnosing Crohn’s Disease
Diagnosing Crohn’s Disease can be challenging because its symptoms often overlap with other gastrointestinal conditions, such as ulcerative colitis, irritable bowel syndrome (IBS), and celiac disease. Since there is no single test that can definitively diagnose Crohn’s, doctors use a combination of medical history, physical examinations, imaging tests, and lab work to confirm the condition.
Early diagnosis is essential for managing inflammation, preventing complications, and improving long-term health outcomes. Below is a breakdown of how Crohn’s Disease is diagnosed and what tests are commonly used.
1. Medical History and Physical Examination
The first step in diagnosing Crohn’s Disease is a thorough review of symptoms, family history, and lifestyle factors. A gastroenterologist may ask:
- When did your symptoms start?
- How frequent and severe are your symptoms (diarrhea, abdominal pain, fatigue, weight loss)?
- Do you have a family history of Inflammatory Bowel Disease (IBD)?
- Have you noticed any triggers, such as certain foods, stress, or medications?
- Do you smoke or have a history of smoking?
During the physical examination, the doctor may check for:
✅ Abdominal tenderness or bloating – Indicating inflammation in the intestines.
✅ Unintended weight loss – A common sign of malabsorption.
✅ Signs of anemia or malnutrition – Such as pale skin or brittle nails.
✅ Swelling or pain in the joints – Since Crohn’s can cause arthritis-related symptoms.
If Crohn’s Disease is suspected, the doctor will recommend further tests to confirm the diagnosis.
2. Laboratory Tests for Crohn’s Disease
Lab tests help assess inflammation levels, nutritional deficiencies, and possible infections that could be causing symptoms.
A. Blood Tests
Bloodwork can reveal:
- Elevated inflammatory markers
- C-reactive protein (CRP) – High levels suggest inflammation.
- Erythrocyte sedimentation rate (ESR) – Measures inflammation in the body.
- Anemia (low red blood cell count) – Often seen in Crohn’s patients due to blood loss or nutrient malabsorption.
- Vitamin and mineral deficiencies – Such as low iron, vitamin B12, or folate, indicating poor absorption.
B. Stool Tests
A stool sample is analyzed to:
- Detect calprotectin or lactoferrin – Proteins indicating intestinal inflammation.
- Rule out bacterial infections or parasites, which can mimic Crohn’s symptoms.
- Check for occult (hidden) blood, suggesting intestinal ulcers or bleeding.
3. Imaging and Endoscopic Tests
If lab results suggest Crohn’s Disease, the next step is imaging and endoscopy to visualize the digestive tract and pinpoint areas of inflammation.
A. Colonoscopy and Endoscopy (Gold Standard for Diagnosis)
- Colonoscopy: A thin, flexible tube with a camera is inserted into the rectum to examine the colon and ileum (last part of the small intestine) for inflammation, ulcers, or strictures.
- Upper Endoscopy: Used if Crohn’s is suspected in the stomach or duodenum (upper GI tract).
- Biopsy: During these procedures, small tissue samples are taken to check for microscopic signs of chronic inflammation, granulomas (clusters of immune cells), or cell damage.
B. MRI and CT Scans
For a more detailed look at the small intestine and deeper layers of the GI tract, doctors may recommend:
- Magnetic Resonance Enterography (MRE) – Uses MRI technology to highlight inflammation, thickened bowel walls, and fistulas (abnormal connections between intestines).
- CT Scan (Computed Tomography) – Provides cross-sectional images of the intestines to detect obstructions, perforations, or abscesses.
C. Capsule Endoscopy
- If standard endoscopy cannot reach affected areas, patients may swallow a tiny wireless camera in a pill-sized capsule, which captures images of the entire small intestine.
- This method is useful for detecting early-stage Crohn’s Disease in the small intestine (ileitis or jejunoileitis).
4. Differential Diagnosis: Ruling Out Other Conditions
Since Crohn’s symptoms overlap with many other diseases, doctors must rule out conditions such as:
❌ Ulcerative Colitis – A similar form of IBD, but it only affects the colon and rectum.
❌ Irritable Bowel Syndrome (IBS) – Causes bloating and diarrhea but lacks chronic inflammation.
❌ Celiac Disease – An autoimmune reaction to gluten that damages the intestines.
❌ Infections (bacterial, viral, parasitic) – Can mimic Crohn’s symptoms but are temporary.
When Should You See a Doctor?
If you experience persistent digestive symptoms, it’s important to seek medical attention early. Warning signs that warrant a doctor’s visit include:
✔️ Chronic diarrhea lasting more than 4 weeks
✔️ Unexplained weight loss and loss of appetite
✔️ Severe abdominal pain and cramping
✔️ Blood in the stool or rectal bleeding
✔️ Fatigue, fever, or joint pain
Early diagnosis and treatment can help prevent complications, such as intestinal strictures, fistulas, or malnutrition. If Crohn’s Disease is confirmed, the next step is exploring treatment options to manage symptoms and prevent flare-ups.
In the next section, we will discuss medications, dietary changes, and therapies available for Crohn’s Disease treatment.
Treatment Options for Crohn’s Disease
While there is no known cure for Crohn’s Disease, the good news is that the condition can be managed with a combination of medications, lifestyle changes, dietary adjustments, and, in some cases, surgical interventions. The goal of treatment is to reduce inflammation, induce remission, and maintain long-term symptom control. This can help patients live relatively normal lives despite the chronic nature of the disease. Below, we’ll explore the various treatment options available for Crohn’s Disease.
1. Medications for Crohn’s Disease
Medications are often the first line of treatment for Crohn’s Disease, and they work by reducing inflammation, controlling symptoms, and preventing flare-ups. The specific medication prescribed depends on the severity of the disease, the part of the digestive tract affected, and the patient’s overall health.
A. Anti-inflammatory Drugs
- Aminosalicylates (5-ASAs) – These medications, such as mesalamine, are used to reduce inflammation in the intestines. They are commonly used for mild cases of Crohn’s Disease or in remission phases to maintain symptom control.
- Corticosteroids (Steroids) – Prednisone and budesonide are effective at reducing inflammation quickly during active flare-ups, but they are typically used for short-term treatment due to potential side effects like weight gain, bone thinning, and high blood pressure.
B. Immunosuppressive Medications
- Thiopurines (e.g., azathioprine, mercaptopurine) – These drugs suppress the immune system to reduce inflammation by blocking the production of immune cells that attack the digestive tract.
- Methotrexate – An immunosuppressant used to manage moderate to severe Crohn’s Disease and help induce remission when other drugs have been ineffective.
C. Biologics
Biologics are advanced targeted therapies that block specific immune system proteins involved in the inflammatory process:
- TNF-alpha inhibitors (e.g., infliximab (Remicade), adalimumab (Humira), certolizumab pegol (Cimzia)) – These drugs block the TNF-alpha protein, a key player in causing intestinal inflammation.
- Integrin inhibitors (e.g., vedolizumab (Entyvio)) – These drugs block the movement of white blood cells to areas of inflammation in the intestines.
- Interleukin inhibitors (e.g., ustekinumab (Stelara)) – These medications target interleukins, which are immune system proteins that promote inflammation.
Biologics are often used for patients who have moderate to severe Crohn’s Disease or those who have not responded to other medications. These drugs are typically administered via injection or infusion and can help maintain long-term remission.
D. Antibiotics
In some cases, antibiotics like metronidazole or ciprofloxacin are prescribed to treat infections or complications such as abscesses or fistulas. However, antibiotics are not a primary treatment for Crohn’s Disease itself.
2. Lifestyle and Dietary Changes
Managing Crohn’s Disease also involves making certain lifestyle and dietary changes to reduce symptoms and avoid flare-ups. While dietary changes can’t cure the disease, they can significantly help in controlling symptoms and improving nutritional status.
A. Crohn’s Disease Diet
What you eat plays a crucial role in managing intestinal inflammation and avoiding symptom exacerbation. Though there’s no one-size-fits-all approach, common dietary strategies include:
- Low-FODMAP Diet: Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) are carbohydrates that can exacerbate symptoms like bloating and diarrhea. A low-FODMAP diet eliminates certain high-fermentable foods like onions, garlic, and dairy to reduce symptoms.
- Gluten-Free Diet: Some people with Crohn’s may find that gluten triggers flare-ups, even though it’s not the cause of the disease. Eliminating gluten-rich foods, such as wheat and barley, may be beneficial.
- High-Protein, Low-Fat, and Easily Digestible Foods: To maintain nutrition, especially during flare-ups, it’s helpful to focus on easily digestible foods such as lean meats, poultry, fish, cooked vegetables, and simple grains like white rice or oats.
- Probiotics: Probiotics (such as Lactobacillus and Bifidobacterium) may help maintain a healthy gut microbiome, which could play a role in managing inflammation. Always consult a doctor before taking probiotic supplements.
B. Stress Management
Although stress doesn’t cause Crohn’s Disease, it can certainly worsen symptoms or contribute to flare-ups. Implementing effective stress management techniques can help reduce the frequency and severity of flare-ups.
- Mindfulness meditation, yoga, and deep breathing exercises can help lower overall stress levels and improve emotional well-being.
- Regular physical activity and adequate sleep also play an important role in managing stress.
3. Surgical Treatments for Crohn’s Disease
In some cases, medications and lifestyle changes are not enough to control symptoms, and surgery may be required. While surgery does not cure Crohn’s Disease, it can help remove damaged portions of the intestine and address complications. Surgery is typically reserved for patients who experience:
- Intestinal blockages (due to strictures).
- Fistulas or abscesses that don’t heal with antibiotics or biologics.
- Severe malnutrition due to an inability to absorb nutrients effectively.
A. Types of Surgery
- Resection – The removal of a diseased section of the intestine, followed by reattaching the healthy ends.
- Strictureplasty – Widening narrowed sections of the intestine without removing any part of it.
- Colectomy – In severe cases, the entire colon may need to be removed, though this is more common in ulcerative colitis than in Crohn’s.
Surgery can help alleviate symptoms and improve quality of life, but recurrence of Crohn’s Disease is still possible, as it can affect other areas of the gastrointestinal tract.
4. Complementary and Alternative Therapies
Some individuals with Crohn’s Disease explore complementary and alternative therapies alongside conventional treatment. These therapies may include:
- Acupuncture to reduce symptoms like pain, nausea, and fatigue.
- Herbal supplements, such as turmeric or aloe vera, which may have anti-inflammatory properties.
- Vitamin and mineral supplements to help with deficiencies (especially iron, vitamin B12, and calcium).
Always consult with a healthcare provider before trying these alternative treatments, as they can interact with medications or have side effects.
Conclusion: Managing Crohn’s Disease
Crohn’s Disease is a chronic condition that can significantly impact an individual’s quality of life, but with early diagnosis, effective treatment, and lifestyle adjustments, it’s possible to manage symptoms and achieve long-term remission. While there is no cure for Crohn’s, medical advancements in medications, biologics, and surgical options have made it easier to control inflammation, reduce flare-ups, and prevent complications.
The journey with Crohn’s Disease requires a multifaceted approach, where managing physical symptoms goes hand-in-hand with addressing emotional and mental well-being. Alongside medical treatments, stress management, proper nutrition, and adequate self-care play pivotal roles in maintaining a balanced and healthy life.
Empowering Self-Management
For many individuals with Crohn’s, learning to manage the disease involves a personalized plan tailored to their unique needs and lifestyle. Patients can feel empowered by:
- Monitoring their symptoms to detect flare-ups early.
- Adopting dietary changes that help reduce gut irritation and maintain nutrition.
- Staying proactive with medication and staying in close communication with their healthcare providers.
- Joining support groups or communities for emotional encouragement and sharing of tips and strategies.
While Crohn’s Disease can be unpredictable, it’s important to remember that advancements in treatment have made it possible to live a full and active life, even while managing a chronic illness. Early intervention, diligent care, and a positive mindset are essential for reducing the frequency of flare-ups and minimizing the impact of the disease.
Long-Term Outlook for Crohn’s Disease
Though Crohn’s Disease is lifelong, the future for individuals diagnosed with this condition is brighter than ever before. Thanks to research and new treatment options, people with Crohn’s can:
- Achieve long-term remission with the right treatment plan.
- Prevent complications such as intestinal strictures, fistulas, and malnutrition, which can lead to more severe health problems.
- Maintain normal daily activities, engage in careers, hobbies, and relationships.
By understanding the disease, committing to a treatment strategy, and adjusting lifestyle habits accordingly, many patients find that Crohn’s Disease becomes more manageable over time.
A Life Beyond Crohn’s Disease
Although Crohn’s Disease will require ongoing care, it doesn’t define a person’s life. With the proper support and resources, individuals can still enjoy a vibrant life and accomplish their personal and professional goals. Living with Crohn’s is about finding balance — between managing the disease, maintaining good physical and mental health, and nurturing relationships and passions.
The key takeaway is that Crohn’s Disease does not have to control your life. With the right mindset, treatment plan, and support network, it’s possible to manage the condition effectively, allowing you to live a fulfilling and productive life.
In conclusion, Crohn’s Disease may be a chronic and complex condition, but with a comprehensive, personalized approach, it is manageable. Keep in mind that regular follow-ups with your healthcare provider, an awareness of your body’s signals, and staying informed about the latest treatment options are all essential tools in navigating this journey. Whether you’re newly diagnosed or have been living with Crohn’s for years, you are not alone in this fight — empower yourself to live life to its fullest.
📚 Recommended Readings and Expert Advice
For those seeking to deepen their understanding of Crohn’s Disease and explore effective management strategies, the following expert-recommended books and articles offer valuable insights:
📘 Top Books on Crohn’s Disease
- Crohn’s and Colitis: Understanding and Managing IBD
Author: Dr. A. Hillary Steinhart
A comprehensive guide blending medical expertise with practical advice on symptom management, medications, and dietary considerations.
Available on Amazon - Listen to Your Gut: The Complete Natural Healing Program for IBS and IBD
Author: Jini Patel Thompson
Offers a holistic approach to gut health, emphasizing natural remedies, dietary modifications, and stress management techniques.
Available on Amazon - The Microbiome Solution: A Radical New Way to Heal Your Body from the Inside Out
Author: Dr. Robynne Chutkan
Explores the role of gut bacteria in digestive health and provides strategies to restore gut balance through diet and lifestyle changes.
Available on Amazon - Tell Me What to Eat If I Have Inflammatory Bowel Disease
Author: Kimberly A. Tessmer
Provides nutritional guidelines and recipes tailored for individuals with Crohn’s Disease and ulcerative colitis.
Available on Amazon - Crohn’s & Colitis Diet Guide: Includes 175 Recipes
Authors: Dr. A. Hillary Steinhart & Julie Cepo, RD
A collaborative effort between a gastroenterologist and a dietitian, offering a plethora of IBD-friendly recipes and dietary advice.
Available on Amazon
📰 Expert Articles and Guides
- Crohn’s Disease Overview – Mayo Clinic
Covers causes, risk factors, complications, and diagnosis.
Read the article - Crohn’s Disease: What You Should Know – CDC
A public health perspective with a focus on prevalence and prevention.
Visit the CDC page - Diet and Nutrition with IBD – Crohn’s & Colitis Foundation
Practical tips for managing symptoms through diet.
Read on Crohn’s & Colitis Foundationأمازون+2cbinsights.com+2أمازون+2 - The First Steps to Managing Crohn’s Disease – Verywell Health
A beginner-friendly guide for newly diagnosed patients.
Read the article - Crohn’s Disease Flare-Up Management – Merus Gastroenterology
A clinical look at managing acute flare-ups and long-term planning.
Read the article - Understanding Symptoms of Crohn’s – Cleveland Clinic
Insightful symptom guide from one of the nation’s leading hospitals.
Visit Cleveland Clinic
These resources are curated to provide comprehensive information and practical strategies for managing Crohn’s Disease effectively. If you need further assistance or personalized recommendations, feel free to ask!