Mental health is a crucial part of overall well-being, yet millions of people worldwide struggle with mental illnesses. These disorders can affect thoughts, emotions, and behaviors, making daily life challenging. According to the World Health Organization (WHO), mental health conditions are among the leading causes of disability, impacting individuals of all ages and backgrounds.
Understanding different types of mental illnesses is essential for early recognition and proper treatment. From mood disorders like depression and bipolar disorder to anxiety disorders such as PTSD and OCD, mental health conditions vary in severity and symptoms. Fortunately, treatments like Cognitive Behavioral Therapy (CBT), medications (SSRIs), and professional counseling can help manage these disorders effectively.
In this article, we will explore a list of 15+ common mental illnesses, their symptoms, and available treatment options. Whether you’re looking to learn more about mental health for yourself or a loved one, this guide provides valuable insights into some of the most prevalent psychological disorders.
- Understanding Mental Illness and Its Impact
- Mood Disorders – The Most Common Mental Health Conditions
- Anxiety and Stress-Related Disorders
- 1. Borderline Personality Disorder (BPD)
- 2. Antisocial Personality Disorder (ASPD)
- 3. Schizophrenia
- 4. Schizoaffective Disorder
- 1. Eating Disorders
- 2. Neurodevelopmental Disorders
- 📚 Recommended Readings and Expert Advice
- 🔗 Sources
Understanding Mental Illness and Its Impact
What is Mental Illness?
Mental illness refers to a wide range of health conditions that affect a person’s thinking, emotions, behavior, and ability to function in daily life. These disorders can be mild, moderate, or severe, and they may be temporary or long-term. According to the American Psychiatric Association (APA), mental illnesses are medical conditions, just like physical illnesses, and they require proper diagnosis and treatment.
Mental health disorders can develop due to a combination of genetic, biological, environmental, and psychological factors. Stressful life events, traumatic experiences, and chemical imbalances in the brain are common contributors.
How Mental Illness Affects Daily Life
The impact of mental illness varies from person to person, but it can disrupt multiple aspects of life, including:
- Emotional Well-being: Persistent feelings of sadness, anxiety, or mood swings.
- Cognitive Functioning: Difficulty concentrating, making decisions, or remembering things.
- Social Relationships: Withdrawal from family and friends, difficulty maintaining personal and professional relationships.
- Work and Productivity: Decreased job performance, absenteeism, or trouble holding employment.
- Physical Health: Increased risk of chronic illnesses like heart disease, weakened immune function, and sleep disturbances.
Mental illness doesn’t just affect the individual—it also impacts families, workplaces, and communities. This is why awareness, early intervention, and professional support are crucial.
The Role of DSM-5 in Diagnosing Mental Illness
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the standard reference used by mental health professionals to diagnose mental illnesses. Published by the American Psychiatric Association (APA), the DSM-5 categorizes disorders based on specific criteria, helping professionals assess symptoms and determine appropriate treatments.
The DSM-5 classifies mental disorders into different categories, including:
- Mood Disorders (e.g., Depression, Bipolar Disorder)
- Anxiety Disorders (e.g., Generalized Anxiety Disorder, Panic Disorder)
- Psychotic Disorders (e.g., Schizophrenia)
- Personality Disorders (e.g., Borderline Personality Disorder)
- Neurodevelopmental Disorders (e.g., ADHD, Autism Spectrum Disorder)
Having a standardized classification system helps ensure accurate diagnoses and effective treatment plans.
The Importance of Seeking Professional Help
Many people with mental health disorders hesitate to seek treatment due to stigma, lack of awareness, or misconceptions about mental illness. However, untreated mental health conditions can worsen over time and lead to severe consequences, including increased risk of substance abuse, self-harm, or suicide.
Seeking help from mental health professionals such as psychiatrists, psychologists, or therapists can make a significant difference. Common treatments include:
- Therapy & Counseling: Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and other evidence-based therapies.
- Medication: Antidepressants, anti-anxiety medications, mood stabilizers, and antipsychotic drugs.
- Lifestyle Changes: Exercise, healthy diet, stress management techniques, and support groups.
Understanding mental illness is the first step toward breaking the stigma and encouraging support. Whether you or someone you know is struggling, resources like the National Alliance on Mental Illness (NAMI) and Mental Health America (MHA) provide valuable guidance and support.
Mood Disorders – The Most Common Mental Health Conditions
Mood disorders are among the most prevalent types of mental illnesses, affecting millions of people worldwide. These conditions primarily impact a person’s emotional state, causing persistent feelings of sadness, extreme mood swings, or emotional instability. According to the World Health Organization (WHO), depression is one of the leading causes of disability globally, highlighting the significant impact of mood disorders on individuals and society.
Below, we explore some of the most common mood disorders, their symptoms, causes, and treatment options.
1. Depression (Major Depressive Disorder – MDD)
Overview:
Depression, or Major Depressive Disorder (MDD), is a serious mental health condition characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities once enjoyed. It can interfere with daily life, work, and relationships.
Symptoms:
- Prolonged sadness or low mood
- Fatigue and low energy levels
- Difficulty concentrating or making decisions
- Changes in appetite and weight
- Sleep disturbances (insomnia or excessive sleep)
- Feelings of worthlessness or guilt
- Thoughts of self-harm or suicide
Causes & Risk Factors:
Depression can be caused by a combination of biological, genetic, psychological, and environmental factors. Traumatic experiences, chronic stress, and imbalances in neurotransmitters (such as serotonin and dopamine) play a role.
Treatment Options:
- Cognitive Behavioral Therapy (CBT): A structured form of talk therapy that helps individuals change negative thought patterns.
- Medication: Antidepressants like Selective Serotonin Reuptake Inhibitors (SSRIs) (e.g., Prozac, Zoloft) can help regulate brain chemistry.
- Lifestyle Changes: Regular exercise, a healthy diet, and mindfulness techniques can improve symptoms.
2. Bipolar Disorder (Manic-Depressive Illness)
Overview:
Bipolar Disorder is a condition that causes extreme shifts in mood, energy, and activity levels. These mood swings range from depressive episodes to manic episodes, where a person experiences heightened energy and impulsivity.
Types of Bipolar Disorder:
- Bipolar I Disorder: Characterized by at least one full manic episode, which may be followed by depressive episodes.
- Bipolar II Disorder: Involves hypomania (a milder form of mania) and major depressive episodes.
- Cyclothymic Disorder: Milder mood swings that do not meet the full criteria for Bipolar I or II.
Symptoms:
- During manic episodes: Increased energy, decreased need for sleep, impulsive behavior, grandiose thoughts.
- During depressive episodes: Low energy, sadness, feelings of hopelessness, suicidal thoughts.
Treatment Options:
- Mood Stabilizers: Medications like lithium or valproate help regulate mood swings.
- Psychotherapy: CBT, Dialectical Behavior Therapy (DBT), and family-focused therapy.
- Lifestyle Adjustments: Establishing a routine, reducing stress, and avoiding triggers like alcohol or substance use.
3. Seasonal Affective Disorder (SAD)

Overview:
Seasonal Affective Disorder (SAD) is a type of depression that occurs seasonally, usually during fall and winter when sunlight exposure decreases. It is believed to be linked to disruptions in the body’s circadian rhythm and a drop in serotonin and melatonin levels.
Symptoms:
- Low energy and fatigue
- Increased sleep and difficulty waking up
- Weight gain and carbohydrate cravings
- Feelings of sadness, hopelessness, or irritability
- Social withdrawal (“hibernation” effect)
Treatment Options:
- Light Therapy (Phototherapy): Using a lightbox that mimics natural sunlight to regulate mood.
- Medication: SSRIs or other antidepressants may be prescribed for severe cases.
- Vitamin D Supplements: Low vitamin D levels have been linked to SAD, so supplementation may help.
4. Persistent Depressive Disorder (Dysthymia)
Overview:
Persistent Depressive Disorder (formerly known as Dysthymia) is a chronic form of depression lasting two years or more. While symptoms may be less severe than major depression, the long-term nature of the condition makes it challenging to manage.
Symptoms:
- Chronic low mood that lasts most of the day
- Low self-esteem and feelings of inadequacy
- Fatigue and low energy
- Difficulty concentrating or making decisions
- Irritability or excessive worry
- Lack of interest in social activities
Treatment Options:
- Psychotherapy: CBT and Interpersonal Therapy (IPT) can help address negative thinking patterns.
- Antidepressant Medication: SSRIs or Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) may be prescribed.
- Behavioral Changes: Exercise, sleep regulation, and stress management techniques.
Mood disorders can significantly impact an individual’s quality of life, relationships, and productivity. However, early diagnosis and proper treatment can make a huge difference. If you or someone you know is struggling with symptoms of a mood disorder, seeking professional help from a psychiatrist or therapist is essential.
Anxiety and Stress-Related Disorders
Anxiety disorders are among the most common mental health conditions, affecting millions of people worldwide. According to the World Health Organization (WHO), anxiety disorders impact over 300 million people, making them one of the leading causes of mental health struggles. While occasional anxiety is a normal response to stress, individuals with anxiety disorders experience excessive and persistent fear, worry, or nervousness that interferes with their daily lives.
Stress-related disorders, such as Post-Traumatic Stress Disorder (PTSD), occur in response to traumatic events, leading to ongoing distress, flashbacks, and emotional instability. These conditions can negatively impact a person’s relationships, work, and overall well-being.
Below, we explore the most common anxiety and stress-related disorders, their symptoms, causes, and treatment options.
1. Generalized Anxiety Disorder (GAD)
Overview:
Generalized Anxiety Disorder (GAD) is characterized by chronic, excessive worry about various aspects of life, such as work, health, or relationships, even when there is no apparent reason to be concerned. This constant state of worry can make it difficult to concentrate, relax, or complete daily tasks.
Symptoms:
- Persistent and uncontrollable worry
- Restlessness or feeling on edge
- Fatigue and difficulty sleeping (insomnia)
- Muscle tension and headaches
- Difficulty concentrating or focusing
- Irritability
Causes & Risk Factors:
GAD can be influenced by genetics, brain chemistry (imbalances in neurotransmitters like serotonin and dopamine), chronic stress, and traumatic experiences.
Treatment Options:
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and challenge negative thought patterns.
- Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) (e.g., Prozac, Zoloft) or Benzodiazepines (for short-term relief).
- Lifestyle Changes: Regular exercise, mindfulness meditation, and relaxation techniques can help reduce symptoms.
2. Panic Disorder
Overview:
Panic Disorder involves sudden and intense episodes of fear, known as panic attacks. These attacks can occur unexpectedly and are often accompanied by physical symptoms that mimic heart attacks, making them extremely distressing.
Symptoms of a Panic Attack:
- Rapid heartbeat (palpitations)
- Shortness of breath or feeling like you’re choking
- Sweating and trembling
- Dizziness or lightheadedness
- Chest pain and nausea
- A feeling of losing control or impending doom
Causes & Risk Factors:
Panic disorder can develop due to genetics, high stress levels, major life changes, or chemical imbalances in the brain. Individuals with a history of trauma are also at higher risk.
Treatment Options:
- Psychotherapy: CBT helps patients recognize triggers and develop coping strategies.
- Medications: SSRIs, Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), or anti-anxiety medications.
- Breathing Techniques & Exposure Therapy: Learning to control breathing and gradually exposing oneself to triggers can help manage panic attacks.
3. Post-Traumatic Stress Disorder (PTSD)
Overview:
Post-Traumatic Stress Disorder (PTSD) is a serious condition that develops after experiencing or witnessing a traumatic event, such as combat, sexual assault, natural disasters, or accidents. PTSD affects both civilians and military veterans and can cause long-term emotional distress and flashbacks.
Symptoms:
- Intrusive thoughts or flashbacks of the traumatic event
- Nightmares and sleep disturbances
- Avoidance behavior (avoiding places, people, or situations that remind them of the trauma)
- Hyperarousal (easily startled, always on edge)
- Emotional numbness or detachment from loved ones
- Guilt, shame, or depression
Causes & Risk Factors:
PTSD occurs when a person fails to process trauma properly, leading to ongoing distress. Brain structure and function also play a role, as PTSD is linked to abnormal activity in the amygdala and hippocampus (brain areas responsible for fear and memory).
Treatment Options:
- Trauma-Focused CBT (TF-CBT): Helps process and reframe traumatic memories.
- Eye Movement Desensitization and Reprocessing (EMDR): A therapy that helps rewire traumatic memories.
- Medication: SSRIs, Prazosin (for nightmares), or anti-anxiety medications.
- Support Groups & Therapy: Connecting with others who have experienced similar trauma can be beneficial.
4. Obsessive-Compulsive Disorder (OCD)
Overview:
Obsessive-Compulsive Disorder (OCD) is a condition where a person experiences persistent, intrusive thoughts (obsessions) that cause anxiety, followed by compulsive behaviors performed to relieve the distress. OCD can interfere with daily life and lead to repetitive rituals that are difficult to control.
Common Obsessions:
- Fear of germs or contamination (excessive handwashing)
- Fear of harming oneself or others (checking locks or appliances repeatedly)
- Need for symmetry or order (arranging objects in a specific way)
- Intrusive, distressing thoughts (religious, violent, or taboo themes)
Common Compulsions:
- Repeated handwashing or excessive cleaning
- Checking things multiple times (e.g., doors, stoves, lights)
- Counting, tapping, or repeating words silently
- Hoarding unnecessary items due to fear of needing them later
Causes & Risk Factors:
OCD is linked to abnormal serotonin levels, genetics, and overactivity in certain brain regions (orbitofrontal cortex and basal ganglia).
Treatment Options:
- Exposure and Response Prevention (ERP): A type of CBT that helps individuals face their fears without performing compulsions.
- Medication: SSRIs such as Fluoxetine (Prozac) or Sertraline (Zoloft).
- Deep Brain Stimulation (DBS): Used in severe, treatment-resistant cases.
Anxiety and stress-related disorders can be overwhelming, but effective treatment is available. Seeking help from mental health professionals such as psychiatrists, psychologists, or therapists can make a significant difference in managing these conditions.
If you or someone you know is struggling with anxiety, panic attacks, PTSD, or OCD, reaching out for therapy, medication, or self-help strategies can lead to improved mental health and a better quality of life.
Personality Disorders and Psychosis
Personality disorders and psychotic disorders are serious mental health conditions that can profoundly affect a person’s emotions, thoughts, behaviors, and relationships. Unlike mood and anxiety disorders, these conditions often involve distorted perceptions of reality, difficulty managing emotions, and problematic interpersonal relationships.
While personality disorders involve persistent, inflexible patterns of thinking and behavior, psychotic disorders involve a loss of touch with reality, such as hallucinations and delusions.
Understanding these disorders is essential for breaking stigma and promoting early diagnosis and treatment. Below, we explore the most common personality disorders and psychotic disorders, their symptoms, causes, and treatment options.
1. Borderline Personality Disorder (BPD)
Overview:
Borderline Personality Disorder (BPD) is a condition characterized by intense emotions, unstable relationships, impulsivity, and self-destructive behaviors. People with BPD often experience a fear of abandonment, extreme mood swings, and difficulty maintaining a stable sense of self.
Symptoms:
- Emotional Instability: Rapid mood changes, intense anger, and feelings of emptiness.
- Unstable Relationships: Alternating between idealizing and devaluing others (“love-hate” relationships).
- Impulsivity & Risky Behaviors: Reckless spending, binge eating, self-harm, or substance abuse.
- Fear of Abandonment: Extreme reactions to perceived or real rejection.
- Dissociation & Paranoia: Feeling detached from reality, especially under stress.
Causes & Risk Factors:
- Genetic & Biological Factors: BPD runs in families and is linked to brain structure differences.
- Childhood Trauma: Abuse, neglect, or unstable family environments increase the risk.
- Environmental Triggers: High-stress situations can worsen symptoms.
Treatment Options:
- Dialectical Behavior Therapy (DBT): A form of therapy that teaches emotional regulation, distress tolerance, and interpersonal effectiveness.
- Cognitive Behavioral Therapy (CBT): Helps manage negative thought patterns.
- Medications: Antidepressants, mood stabilizers, or antipsychotic medications may help with symptoms.
- Support Systems: Therapy groups and a strong support network are crucial for managing BPD.
2. Antisocial Personality Disorder (ASPD)
Overview:
Antisocial Personality Disorder (ASPD) is characterized by a lack of empathy, disregard for rules and social norms, and manipulative or harmful behavior. People with ASPD may engage in criminal activity, deceit, or reckless behavior without remorse.
Symptoms:
- Manipulative & Deceptive Behavior: Persistent lying and exploiting others.
- Disregard for Social Norms: Engaging in illegal activities or reckless behavior.
- Lack of Empathy & Remorse: Inability to feel guilt for harming others.
- Impulsivity & Aggressiveness: Prone to violent outbursts or risky behaviors.
Causes & Risk Factors:
- Genetics & Brain Differences: ASPD is linked to reduced activity in the prefrontal cortex, which controls decision-making and impulse control.
- Childhood Trauma: Early exposure to violence, neglect, or abuse increases risk.
- Environmental Factors: Growing up in unstable or criminal environments can contribute.
Treatment Options:
- Cognitive Behavioral Therapy (CBT): Helps individuals recognize destructive behavior patterns.
- Group Therapy & Social Support: Can improve interpersonal skills.
- Medication: There is no specific medication for ASPD, but mood stabilizers and antidepressants may help control aggression.
3. Schizophrenia
Overview:
Schizophrenia is a severe psychotic disorder that affects a person’s ability to think clearly, manage emotions, and interact with others. It is often misunderstood and stigmatized, despite being a treatable condition.
Symptoms:
- Hallucinations: Seeing, hearing, or feeling things that are not real (most commonly auditory hallucinations).
- Delusions: Strong, false beliefs that contradict reality (e.g., believing they are being controlled by external forces).
- Disorganized Thinking & Speech: Trouble organizing thoughts, speaking in a way that is hard to follow.
- Emotional & Social Withdrawal: Lack of motivation, reduced speech, and difficulty forming relationships.
- Cognitive Impairments: Struggles with memory, problem-solving, and concentration.
Causes & Risk Factors:
- Genetics: Schizophrenia often runs in families.
- Brain Chemistry & Structure: Imbalances in dopamine and abnormal brain development.
- Environmental Triggers: Stress, trauma, or drug use (e.g., cannabis use in adolescence) may trigger symptoms.
Treatment Options:
- Antipsychotic Medications: Clozapine, Risperidone, and Olanzapine help manage symptoms.
- Psychotherapy & Rehabilitation: Cognitive therapy and social training help improve daily functioning.
- Hospitalization & Support Services: For severe cases, inpatient care may be needed.
4. Schizoaffective Disorder
Overview:
Schizoaffective Disorder is a mental health condition that combines symptoms of schizophrenia (psychosis) and mood disorders (depression or bipolar disorder). It is often misdiagnosed as either schizophrenia or bipolar disorder alone.
Symptoms:
- Psychotic Symptoms: Hallucinations and delusions (similar to schizophrenia).
- Mood Disorder Symptoms: Depressive episodes, manic episodes, or both.
- Disorganized Thinking & Behavior: Confusion, erratic speech, or difficulty completing tasks.
Causes & Risk Factors:
- Genetic & Brain Chemistry Factors: Similar to schizophrenia and bipolar disorder.
- Environmental Triggers: Stress, trauma, and substance use.
Treatment Options:
- Antipsychotic & Mood Stabilizing Medications: To manage both psychosis and mood symptoms.
- Therapy & Support Programs: CBT, family therapy, and peer support can improve quality of life.
Personality disorders and psychotic disorders can be challenging to diagnose and treat, but early intervention and proper management can lead to better outcomes. If you or someone you know is experiencing symptoms, seeking help from a psychiatrist, psychologist, or therapist is crucial.
With therapy, medication, and lifestyle adjustments, individuals with these disorders can lead fulfilling lives. If you suspect you or a loved one may have a personality or psychotic disorder, reach out to mental health professionals or support organizations like NAMI (National Alliance on Mental Illness) for guidance.
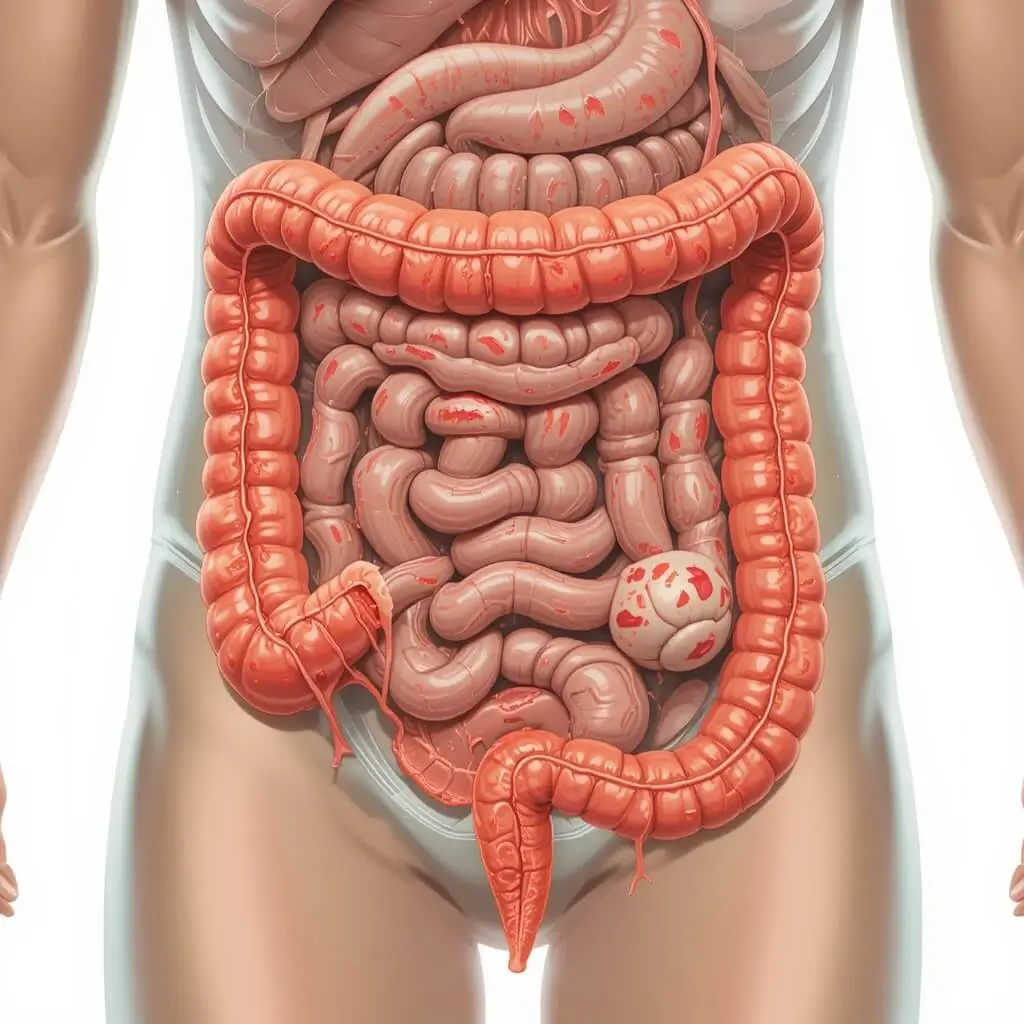
Eating Disorders and Neurodevelopmental Disorders
Eating disorders and neurodevelopmental disorders are distinct yet equally significant mental health conditions that affect millions of people worldwide.
- Eating disorders are characterized by abnormal eating habits, extreme concern with body weight, and unhealthy relationships with food. These disorders can lead to severe physical and psychological health complications if left untreated.
- Neurodevelopmental disorders involve brain development differences that affect cognition, behavior, and social interactions. They are often diagnosed in childhood but can persist into adulthood.
Understanding these disorders is essential for early intervention and effective treatment. Below, we explore the most common eating disorders and neurodevelopmental conditions, their symptoms, causes, and treatment options.
1. Eating Disorders
1.1 Anorexia Nervosa
Overview:
Anorexia Nervosa is an eating disorder marked by intense fear of gaining weight, severe calorie restriction, and a distorted body image. Despite being underweight, individuals with anorexia often perceive themselves as overweight.
Symptoms:
- Extreme weight loss or refusal to maintain a healthy weight
- Fear of weight gain despite being underweight
- Excessive exercise or restrictive eating habits
- Distorted body perception (seeing oneself as overweight when they are not)
- Malnutrition-related complications (brittle hair, osteoporosis, heart problems)
Causes & Risk Factors:
- Genetic factors: Family history of eating disorders increases risk
- Psychological factors: Perfectionism, low self-esteem, or past trauma
- Cultural pressures: Media portrayal of thinness as an ideal

Treatment Options:
- Nutritional rehabilitation & therapy (working with dietitians and mental health professionals)
- Cognitive Behavioral Therapy (CBT): Addresses distorted body image and unhealthy behaviors
- Medical intervention: For severe cases, hospitalization may be required to address malnutrition
1.2 Bulimia Nervosa
Overview:
Bulimia Nervosa involves episodes of binge eating followed by purging behaviors such as vomiting, excessive exercise, or laxative use to prevent weight gain. Individuals with bulimia often feel out of control when eating and experience extreme guilt afterward.
Symptoms:
- Frequent binge-eating episodes followed by purging behaviors
- Intense fear of weight gain
- Damaged teeth & gums due to frequent vomiting
- Dehydration, electrolyte imbalances, and digestive issues
Causes & Risk Factors:
- Low self-esteem & perfectionism
- History of trauma or emotional distress
- Social pressure to maintain a certain body weight
Treatment Options:
- CBT and psychotherapy: Helps break the binge-purge cycle
- Nutritional counseling: Establishing healthy eating patterns
- Medication: Antidepressants (like Fluoxetine) may help with impulse control
1.3 Binge-Eating Disorder (BED)
Overview:
Binge-Eating Disorder (BED) is the most common eating disorder, characterized by frequent overeating without compensatory purging behaviors. Unlike bulimia, individuals with BED do not try to rid their bodies of calories through vomiting or excessive exercise.
Symptoms:
- Recurrent binge-eating episodes (eating large quantities of food in a short time)
- Feelings of guilt, shame, or distress after eating
- Eating even when not hungry
- Weight gain or obesity-related health issues
Causes & Risk Factors:
- Emotional triggers: Stress, depression, or anxiety
- Dopamine imbalances: BED may be linked to the brain’s reward system
- Genetic predisposition
Treatment Options:
- CBT & therapy: To address emotional eating patterns
- Nutritional counseling & mindful eating strategies
- Medication: Vyvanse (Lisdexamfetamine) may be prescribed for severe BED cases
2. Neurodevelopmental Disorders
2.1 Attention-Deficit/Hyperactivity Disorder (ADHD)
Overview:
ADHD is a neurodevelopmental disorder that affects focus, impulse control, and hyperactivity. It can persist into adulthood, affecting academic, professional, and personal life.
Symptoms:
- Inattention: Difficulty focusing, forgetfulness, easily distracted
- Hyperactivity: Restlessness, inability to sit still, excessive talking
- Impulsivity: Acting without thinking, interrupting others, difficulty waiting for turns
Causes & Risk Factors:
- Genetics: Strong hereditary component
- Brain chemistry: Differences in dopamine regulation
- Environmental factors: Premature birth, lead exposure, or prenatal alcohol exposure
Treatment Options:
- Behavioral therapy: Helps with focus and impulse control
- Medications: Stimulants (Adderall, Ritalin) or non-stimulants (Strattera)
- Lifestyle modifications: Exercise, structured routines, and mindfulness techniques
2.2 Autism Spectrum Disorder (ASD)
Overview:
Autism Spectrum Disorder (ASD) is a developmental condition that affects communication, social interaction, and behavior. Symptoms vary widely, from mild to severe.
Symptoms:
- Social difficulties: Difficulty understanding emotions, eye contact avoidance
- Repetitive behaviors: Hand-flapping, rocking, or strict routines
- Sensory sensitivities: Over- or under-reaction to sounds, textures, or lights
Causes & Risk Factors:
- Genetic factors: Strong hereditary link
- Brain structure differences: Variations in neural connectivity
- Environmental factors: Advanced parental age, prenatal infections, or low birth weight
Treatment Options:
- Applied Behavior Analysis (ABA): Structured therapy to improve communication and social skills
- Speech & occupational therapy: Helps with language and motor skills
- Medications: To manage anxiety, ADHD symptoms, or sleep issues
2.3 Learning Disabilities (Dyslexia, Dyscalculia, Dysgraphia)
Overview:
Learning disabilities affect reading, writing, and math skills despite normal intelligence. They are often diagnosed in childhood.
Common Types:
- Dyslexia: Difficulty reading and interpreting words
- Dyscalculia: Difficulty understanding numbers and math concepts
- Dysgraphia: Trouble with writing and fine motor coordination
Treatment Options:
- Specialized education plans (IEPs)
- Speech & occupational therapy
- Assistive technology for learning
Both eating disorders and neurodevelopmental disorders require early diagnosis and treatment to prevent long-term consequences.
- If you or someone you know is struggling with disordered eating, seeking help from mental health professionals, dietitians, or support groups can lead to recovery.
- For neurodevelopmental disorders, early intervention programs, therapy, and educational support can help individuals thrive.
If you suspect an eating disorder or neurodevelopmental condition, reach out to a licensed professional for proper assessment and treatment options.
Conclusion: The Importance of Mental Health Awareness and Support
Mental illnesses are diverse, complex, and often misunderstood, affecting millions of people worldwide. From mood disorders and anxiety conditions to psychotic disorders and neurodevelopmental challenges, mental health conditions vary in severity but share a common need for awareness, early intervention, and proper treatment.
Key Takeaways from This Guide
- Mental health disorders are real and treatable. Conditions like depression, anxiety, schizophrenia, and eating disorders are not just personal weaknesses or character flaws—they are legitimate medical conditions that require professional care.
- Early diagnosis and treatment are crucial. The sooner a person seeks help, the better the chances of managing symptoms and improving quality of life.
- Stigma and misinformation can prevent recovery. Many people avoid seeking help due to fear of judgment, but mental health should be treated like physical health—with compassion and support.
- A strong support system makes a difference. Family, friends, therapists, and support groups play a crucial role in helping individuals cope with mental health challenges.
- Holistic well-being is essential. Mental health is closely linked to physical health, lifestyle habits, social relationships, and self-care practices.
Seeking Help: When and Where to Start
If you or someone you know is struggling with mental health issues, reaching out for support is the first and most important step. Here’s how:
✅ Consult a mental health professional (psychiatrist, psychologist, or therapist) for evaluation and guidance.
✅ Explore therapy options such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), or group therapy.
✅ Consider medication if recommended by a healthcare provider.
✅ Join support groups (e.g., NAMI, Mental Health America) to connect with others who understand.
✅ Practice self-care, including a balanced diet, exercise, mindfulness, and stress management.
Final Thought: You Are Not Alone
Mental health struggles can feel overwhelming, but help is available, and recovery is possible. No matter how difficult things may seem, you deserve support, understanding, and a path to healing.
By increasing awareness and fostering open conversations about mental health, we can help break the stigma, support those in need, and create a healthier society where mental well-being is prioritized.
If you or someone you love is facing a mental health crisis, don’t hesitate to reach out to a mental health professional or crisis hotline for immediate help.
Next Steps
For more insights on mental wellness, coping strategies, and treatment options, explore our related articles on:
🔹 How to Recognize the Early Signs of Mental Illness
🔹 Best Therapy Approaches for Managing Mental Health Disorders
🔹 Self-Care Strategies to Improve Mental Well-being
Let’s continue the conversation—mental health matters, and so do you.
📚 Recommended Readings and Expert Advice
To deepen your understanding of mental health, check out these expert-backed resources and recommended readings:
1. Understanding Mental Illness
- Article: Mental Illness Basics – National Institute of Mental Health (NIMH)
- Summary: An excellent starting point to learn about different types of mental disorders, symptoms, and treatments from a scientific perspective.
2. Treatment Options and Therapy
- Article: Types of Mental Health Treatments – Mayo Clinic
- Summary: Explore various treatment types such as psychotherapy, medications, and lifestyle changes recommended by experts.
3. Recognizing Early Signs
- Article: Warning Signs of Mental Illness – Mental Health America
- Summary: Learn how to identify early warning signs in yourself or others, a critical step in prevention and early intervention.
4. Living with Mental Illness
- Article: Living Well with Mental Illness – National Alliance on Mental Illness (NAMI)
- Summary: Real stories and expert strategies to help individuals manage their mental health conditions and thrive.
5. Expert Podcast & Video Resources
- Podcast: The Happiness Lab by Dr. Laurie Santos
- Video: TED Talk: “There’s No Shame in Taking Care of Your Mental Health” by Sangu Delle
🔗 Sources
Below are the reputable sources used throughout this article: